If you’ve ever shut down a case of the sniffles with cold medicine, had an antibiotic prescribed for an infection or hiked up your sleeve for a vaccine, it’s only because that treatment endured a long, thorough research process. Clinical trials are the gold standard for determining the benefits and harms of any health intervention, says Dr. Jonathon Maguire, a pediatric scientist in the Li Ka Shing Knowledge Institute of St. Michael’s Hospital in Toronto. “We want the health care system to be as strong as it can be and for the risks of health interventions to be as low as possible—and for that, we need clinical trials.”
Month: November 2021
Bookings for pediatric COVID-19 vaccine appoints now open – how can we ensure an equitable rollout?
Global News AM 640 Toronto – The Kelly Cutrara Show
MAP Investigator and St. Michael’s Hospital pediatrician Dr. Shazeen Suleman spoke with AM 640 Radio about Ontario’s pediatric COVID-19 vaccine rollout.
“When we are thinking about vaccines, we want to make sure that every single child and family who wants to get them, can get them. And that means we need to think about accessibility for both the child and their caregivers… Making sure that parents and providers can actually get their child to vaccine sites. So, for example, thinking about how paid sick days are important for parents and caregivers to be able to stay home with their child, after they’ve had their vaccine, or take them to the vaccine clinic. Making sure that clinic hours are perhaps extended, or after hours or on weekends. Thinking about having childcare onsite – we’ve got lots of families that are single parents, and have multiple children, what are they going to do when they have other children that they need to take care of, and take their child to get vaccinated? And also thinking about how we can convey our information in an accessible and equitable way. Making sure language and our communications are done in a way that all families can understand, and interpreted in languages that families may use… Making sure its accessible to families that don’t have health insurance. These are some ideas – and I’ve given you a lot – to think about how we can make it more equitable.”
Il est désormais possible de prendre rendez-vous pour obtenir le vaccin pédiatrique contre la COVID-19; comment pouvons-nous assurer un déploiement équitable?
Global News AM 640 Toronto – The Kelly Cutrara Show
Chercheuse au MAP et pédiatre à l’hôpital St. Michael, la Dre Shazeen Suleman a accordé une entrevue à la radio AM 640 au sujet du déploiement du vaccin pédiatrique contre la COVID-19 en Ontario.
« Quand nous pensons aux vaccins, nous voulons nous assurer que tous les enfants et toutes les familles qui le souhaitent peuvent y avoir accès. Nous devons donc envisager l’accessibilité, tant pour les enfants que pour les personnes qui s’en occupent… Veiller à ce que les parents et les dispensateurs de soins aient la possibilité d’amener leur enfant sur les lieux de vaccination. Par exemple, nous avons réfléchi à l’importance des congés de maladie payés afin de permettre aux parents et aux dispensateurs de soins de rester à la maison avec l’enfant après la vaccination ou de l’emmener à la clinique de vaccination. S’assurer que les heures d’ouverture des cliniques peuvent être prolongées, voire en dehors des heures d’ouverture ou pendant les week-ends. Envisager la mise en place d’un service de garde sur place; nous avons beaucoup de familles monoparentales qui ont plusieurs enfants, que vont-elles faire lorsqu’elles ont d’autres enfants dont elles doivent s’occuper et qu’elles doivent emmener l’un d’eux se faire vacciner? Nous réfléchissons également à la manière dont nous pouvons transmettre nos informations de manière accessible et équitable. S’assurer que la langue et nos communications sont formulées de façon à ce que toutes les familles puissent les comprendre, et qu’elles sont traduites dans des langues que les familles sont susceptibles de maîtriser… S’assurer qu’elles sont accessibles aux familles qui n’ont pas d’assurance maladie. Ce sont là plusieurs idées auxquelles nous pouvons réfléchir afin de rendre le processus plus équitable. »
Vaccinating Ontario Kids Against COVID-19
From TVO The Agenda with Steve Paikin
Featuring Tara Kiran
This week the Ontario government announced children age of five to 11 will be eligible to get their vaccinations. As they and their parents prepare for their first dose, we look at what the roll out will look like, examine infections amongst children in the province, and evaluate parental worries. Is this the light at the end of the pandemic tunnel?
Dr. Sharmistha Mishra’s #OneBurningQuestion: What drives pandemics and why?
Dr. Sharmistha Mishra’s research has shown deep inequities in the spread of COVID-19 and the response to the virus. For her, it’s personal.
“You can see your uncles and aunties in the patients you look after, in the data that you’re working with,” she says. “With most of my family living in India and also affected, the underlying social and structural context of transmission was hard to miss.”
Dr. Mishra, a scientist at MAP Centre for Urban Health Solutions and an Infectious Diseases physician at St. Michael’s, works with her team to get at the “why” of the COVID-19 pandemic. Why is transmission more prominent in some neighbourhoods and networks? Why do some forms of essential work correlate with higher rates of COVID-19? Why have the impacts of the pandemic and the benefits of public health measures been inequitably distributed?
In three recent studies, one about COVID-19 cases and deaths among essential workers in Toronto; one about how variants of concern concentrated where previous variants had similarly clustered; and a third about increased cases of COVID-19 by socioeconomic factors and geography, Dr. Mishra and her colleagues tackle the role of social determinants of health in the pandemic and its response head-on.
To that end, the team has also developed methods to help generate more nuanced mathematical models. These models aim to capture the sources of similarity and of differences between transmission contexts and the extent to which a failure to address underlying context undermines the anticipated impact of a public health response.
Questions à un scientifique du MAP : Qu’est-ce qui est à l’origine des pandémies et quelles sont les raisons de leur apparition?
Les recherches de la Dre Sharmistha Mishra ont révélé de profondes inégalités dans la propagation de la COVID-19 et dans la réaction au virus. Pour elle, la question est personnelle.
« Vous reconnaissez vos oncles et vos tantes dans les patients dont vous vous occupez, dans les données avec lesquelles vous travaillez », dit-elle. « Comme la plupart des membres de ma famille vivent en Inde et sont également touchés, le contexte social et structurel sous-jacent de la transmission me semblait évident. »
Scientifique au Centre MAP pour des solutions de santé urbaine et médecin spécialiste des maladies infectieuses à l’hôpital St. Michael, la Dre Mishra travaille avec son équipe à comprendre le « pourquoi » de la pandémie de COVID-19. Pourquoi la transmission est-elle plus importante dans certains quartiers et au sein de certains réseaux? Pourquoi y a-t-il une corrélation entre certains types de travail essentiel et des taux plus élevés de COVID-19? Pour quelles raisons les impacts de la pandémie et les bienfaits résultant des mesures de santé publique sont-ils répartis de manière inéquitable? Selon trois études récentes (l’une portant sur les cas et les décès de COVID-19 parmi les travailleurs essentiels à Toronto, l’autre sur la manière dont des variants préoccupants se sont manifestés là où les variants précédents s’étaient regroupés de manière similaire, et la troisième concernant l’augmentation des cas de COVID-19 selon les facteurs socio-économiques et géographiques), la Dre Mishra et ses collègues abordent de front le rôle des déterminants sociaux de la santé dans le contexte de la pandémie et de ses conséquences.
It’s time to put down the phone and see your doctor in person, physicians say
Is it time to go back to the doctor’s office?
“If you have a chronic condition like high blood pressure or diabetes, it’s important to measure your blood pressure on an ongoing basis,” said Dr. Tara Kiran, an associate professor at the Temerty School of Medicine and a family doctor at St. Michael’s Hospital. “Even if you have your own machine at home, it’s really important to come and see your doctor every year so that we can make sure the readings are the same as the ones in the office.”
“In my own practice, I’ve found it helpful to see people in person if they have mental health concerns,” said Kiran. “Sometimes you can have a good therapeutic relationship over the phone or on video but part of the recovery process is building that relationship and connecting with people.”
She continued: “I think your doctor is more likely to be there, paying attention and connecting with you, if you’re in person, just the way all humans would be.”
‘There is a lot of fuel’ for COVID: Ontario vaccine data shows big lags in some areas, demographic groups
As Ontario slowly creeps toward the goal of having 90 per cent of the eligible population vaccinated against COVID-19, new data shows vaccine rates are stubbornly lagging in some neighbourhoods and among groups of people across the province.
For Dr. Stephen Hwang, a physician and research scientist at St. Michael’s Hospital and the MAP Centre for Urban Health Solutions, the low vaccine uptake among the homeless population points to a need for outreach beyond just the shelter system, such as visiting supervised drug injection sites.
Among Ontarians who have recently experienced homelessness, only 45 per cent between ages 12 and 64 are fully vaccinated, while 65 per cent over age 65 have had two shots.
“People experiencing homelessness are going to have multiple barriers to getting vaccinated,” Hwang said. They often don’t have internet access, for example, and can’t look up where to go for a shot.
They also may have some hesitation getting vaccinated due to distrust of the health-care system, government or authority figures.
“The other thing would be competing priorities, if someone is figuring out their basic survival needs, getting a vaccination may not be a high priority,” he added.
There are growing calls for drug decriminalization. Could it solve Canada’s opioid crisis?
Experts say decriminalization of drug possession can help tackle the overdose opioid crisis, but it’s not enough and additional measures are needed.
Daniel Werb, director of the Center on Drug Policy Evaluation at St. Michael’s Hospital in Toronto, said Canada’s highest priority should be to regulate its drug market.
“Decriminalization is not going to directly influence overdose mortality,” he said. “The way to directly reduce overdose mortality is by regulating the drug supply.”
Policing practices and threshold limits are other issues to consider to ensure inequities are not amplified by drug policies, said Werb.
“It’s about maximizing the benefits of this policy change by making sure that there aren’t other factors or other policing patterns that come into play that essentially make it the status quo for some people who use drugs,” he said.
Increase in minimum wage good, but not good enough, experts say
As of Jan. 1, the $14.35-an-hour minimum wage will jump to $15. Dr. Shazeen Suleman, pediatrician at St. Michael’s Hospital and member of the Decent Work and Health Network, joins CBC Radio Ontario Today and explains the link between health and basic income, and what the increase means for “the one in five children in Ontario living in poverty.”
Interview with Dr. Shazeen Suleman at 34:30
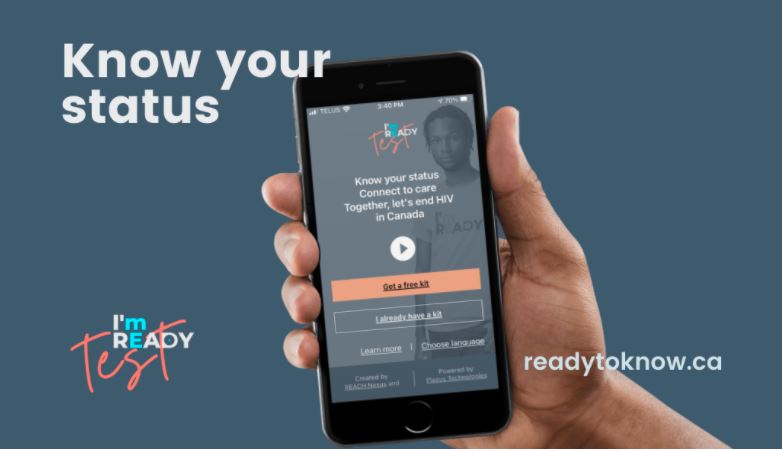
I’m Ready HIV self-testing research program releases its first data summary
Data from June through August 2021 shows promising uptake of the program among key populations and includes 3 positive test results
The I’m Ready research program’s first-ever data summary, for the program’s first quarter, is now available .
Launched in June 2021, I’m Ready invites people to download its I’m Ready, Test app to join the program, after which they can order up to three free HIV self-test kits for delivery or to be picked up at over 80 participating locations across Canada . Critically, participants are also supported to connect to care and prevention, either on their own using this website’s Care pathways , or by booking an appointment with the program’s peer navigators for support before, during or after they self-test for HIV.
The first-quarter data summary , which captures participant data from June through August 2021, highlights the following key findings:
● 14,000+ website visitors;
● 1,579 people consented and entered the study through the I’m Ready, Test app;
● 1,311 participants started the pre-test survey;
● 1,100 participants ordered 2,653 HIV self-test kits for delivery or pick up;
● 496 participants added at least one test result in the app; and
● 3 positive test results submitted, all from key populations.
Noted Dr. Sean B. Rourke, I’m Ready’s Principal Investigator, Director of REACH Nexus and Scientist with MAP Centre for Urban Health Solutions, “Collecting data in real-time is critical to understanding what is and isn’t working so we can continue to improve our program and make a difference—particularly for key populations who are most affected by health inequities.”