Physicians and outreach workers at St. Michael’s Hospital are seeing an alarming rise in the number of homeless individuals coming to the emergency department seeking shelter and suffering from severe cold-related injuries, including frostbite, painful foot infections and life-threatening hypothermia.
Hospital staff say the crisis has escalated in the last two weeks due to a critical lack of space in the city’s shelter system, hit hard by the Omicron variant.
At St. Michael’s Hospital’s emergency department, about 20 per cent of its patient visits are by patients experiencing homelessness, said Dr. Carolyn Snider, chief of emergency medicine at the hospital, a part of Unity Health Toronto. And while the ER does see an increase in the number of underhoused individuals seeking care in the winter, the recent spike caused by Omicron hitting the shelter system alongside frigid temperatures is different, she said.
“We’re seeing more patients. They’re staying longer because there is nowhere else to send them. And they’re coming in sicker, with more cold-related injuries.”
Hospital staff are seeing cases of “trench foot” in underhoused patients. The serious condition is caused when feet are cold and wet for too long. “Their socks are wet, their feet have been in the cold and snow, and their skin is macerated from that,” Snider said, adding that if left untreated patients can get serious infections.
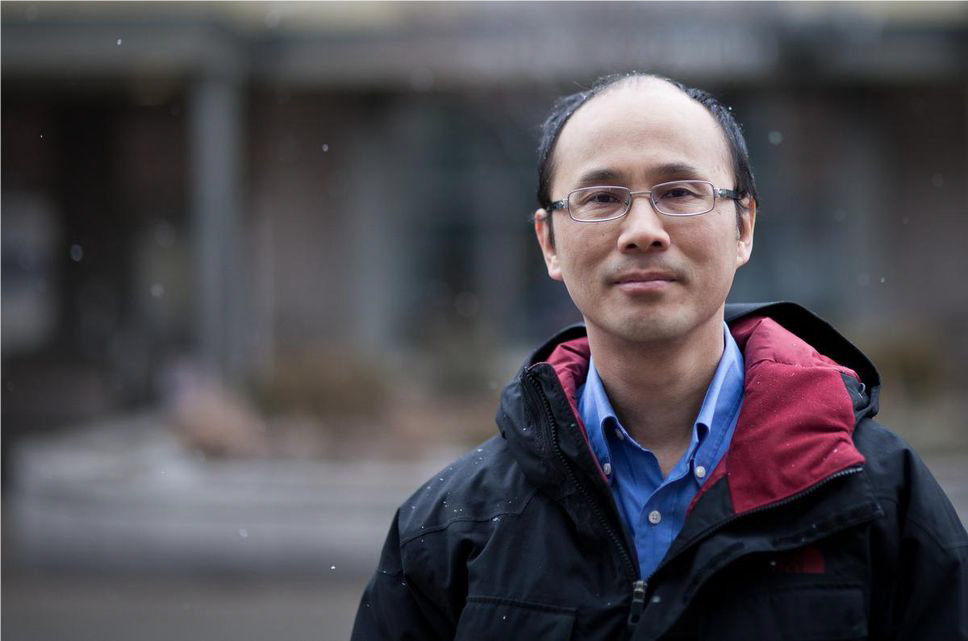
Dr. Stephen Hwang, director of the MAP Centre for Urban Health Solutions, said the recent experiences of St. Mike’s staff offer a window into what is happening in the shelter system and points to the immediate need for more warming centres and more shelter beds.
He noted that some city shelters experiencing a COVID outbreak are directed to not accept new clients for public health reasons, a decision that may be causing additional harm. According to SSHA, some locations can continue accepting clients with appropriate protections and under guidance from Toronto Public Health. And while in some cases shelters may need to close for a short time, “all efforts are being dedicated to ensure access to safe indoor spaces for people in need,” SSHA said.
Hwang, a physician at the hospital and a researcher who studies homelessness and health, said given the current shelter pressures and extreme cold, he hoped city staff would see the importance of offering a person shelter from the cold. “The need for more shelter beds right now in the city, we are seeing it from a health-care perspective. But we know people in the community are seeing it every day as well. We are all very concerned.”