Hayley Thompson of Ontario’s Drug Checking Community, spoke to the CBC about powerful drugs used primarily by veterinarians to sedate animals increasingly showing up in Toronto’s unregulated drug supply.
Author: Samira Prasad
Thunder Bay advocates push for emergency declaration over homelessness
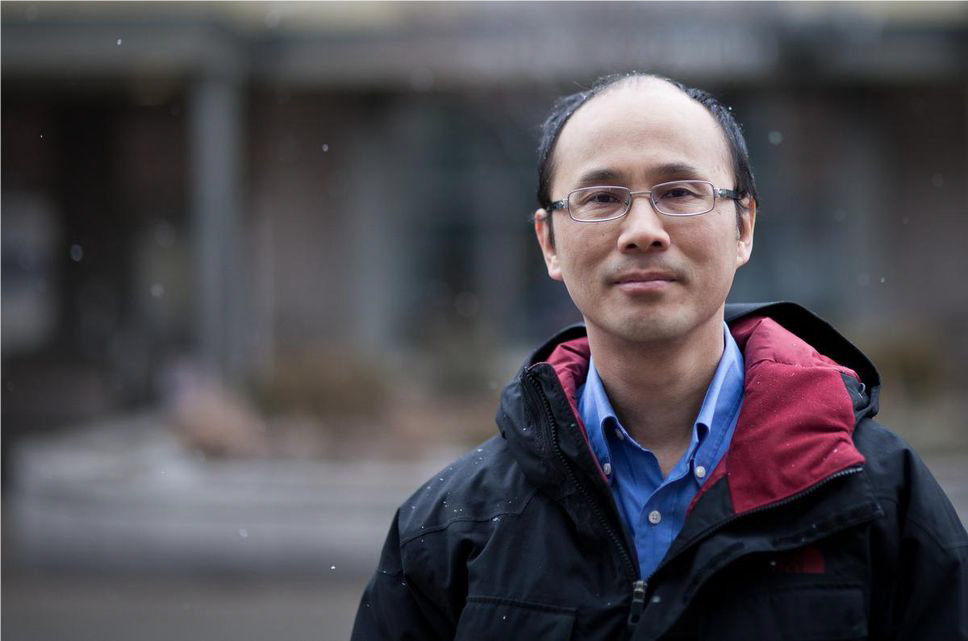
MAP director and scientist Dr. Stephen Hwang, spoke to CBC News in Thunder Bay for a story about a possible state of emergency over homelessness in the community. Housing advocates and Indigenous leaders in Thunder Bay, Ont., have been calling on the city to declare a state of emergency over homelessness, while city staff are pushing for a humanitarian crisis to be declared, instead.
Oral HIV self-test approved for sale, advocates say it’s key to elimination
Dr. Sean Rourke spoke with The Canadian Press about a new oral, at-home HIV test that delivers results in as little as 20 minutes. The test has been used in the U.S. for well over a decade is finally coming to Canada. Rourke said his team at St. Mike’s will start taking orders in the coming weeks from health providers, front-line agencies and hopefully, governments.
“This is the gap that we’ve been missing to reach the people who need it the most,” Rourke said, speaking about communities that are at increased risk as a result of health inequities.
This piece was also published on Global News.
New study from REACH Nexus and Black-led health organizations aims to boost PrEP in Black Communities
TORONTO – REACH Nexus, based at the MAP Centre for Urban Health Solutions at St. Michael’s Hospital (Unity Health Toronto), has partnered with three Black-led community health organizations to launch a new study aimed at improving access to the HIV prevention medication PrEP (pre-exposure prophylaxis) for African, Caribbean, and Black communities in the Greater Toronto Area.
The study, called the Safe Steps Model, is being conducted by REACH along with TAIBU Community Health Centre (TAIBU CHC), the Black Coalition for AIDS Prevention (Black CAP), and Africans in Partnership Against AIDS (APAA), along with other clinical and social service providers. Together, these organizations provide culturally safe care and wellness programming for Black communities across the GTA.
Dr. Wale Ajiboye, adjunct scientist with REACH Nexus, and project lead for Safe Steps, said the study team is using community engagement and culturally responsive care to tackle longstanding barriers to PrEP access, including stigma, limited service access, and anti-Black racism in the health system.
“The Safe Steps Model is culturally responsive, grounded in protection motivation and self-determination theory, and designed to address key individual and systemic barriers to using HIV prevention tools,” said Dr. Ajiboye. “This study has the potential to significantly expand prevention efforts and improve health outcomes for those at risk.”
The study is now enrolling participants to address individual, social, and structural barriers to HIV prevention. It emphasizes client independence, relationship-building, and access to essential resources, like social services, that help address the underlying social determinants of health and support people in meeting their HIV prevention goals.
PrEP—taken orally or as an injectable—prevents HIV acquisition and is a central strategy in Canada’s goal of reaching zero new HIV infections by 2030. Yet uptake remains low among African, Caribbean, and Black communities. In Ontario, Black residents represent 5.5% of the population but accounted for 25% of new HIV diagnoses in 2020 (Ontario HIV Surveillance Initiative). Ongoing medical mistrust, rooted in systemic racism, continues to limit access to care.
“TAIBU is excited to lead this important study that aims to create a more equitable and accessible path to HIV prevention and help dismantle the barriers created by anti-Black racism,” said Liben Gebremikael, Chief Executive Officer of TAIBU CHC. “Everyone, regardless of their background, should have what they need to protect their health.”
The study aims to reduce these disparities by supporting informed, equitable access to HIV prevention while addressing broader social determinants of health.
“Our collaboration with the Safe Steps Project reinforces APAA’s longstanding commitment to community-based leadership in the HIV response,” said APAA executive director Fanta Ongoiba.
“Together, we are building stronger pathways to care that respect the lived experiences, voices, and priorities of ACB communities.”
A recent study co-led by researchers at St. Michael’s Hospital found that Black men were 66% less likely than white men to be aware of PrEP. Among participants in rural areas, Black men were also about 60% less likely to be using PrEP compared to white men.
The findings underscored the urgent need for targeted, culturally relevant interventions to ensure equitable access to HIV prevention across Canada.
“Black CAP is proud to partner on the Safe Steps Program to expand HIV prevention access in our communities. Culturally grounded, community-led approaches like the Safe Steps Program are essential to reducing new infections and ensuring Black individuals can make informed, empowered decisions about their health,” said Elizabeth Mutinda, Executive Director of Black CAP.
About REACH Nexus
REACH Nexus is a national research group working to end HIV, Hepatitis C, and other STBBIs in Canada. A part of the MAP Centre at St. Michael’s Hospital, REACH focuses on reaching the undiagnosed, scaling up testing, improving access to prevention (PrEP and PEP), connecting people to care, and ending stigma. It partners with people living with HIV, service providers, community organizations, public health, industry, and policymakers. Follow REACH on Twitter, Instagram, and Facebook.
About TAIBU Community Health Centre
TAIBU, meaning “Be in Good Health” in Kiswahili, is a community health centre serving Black-identifying residents of the Greater Toronto Area. TAIBU offers primary care, health promotion, and disease prevention services in a culturally affirming environment tailored to address the needs of marginalized populations facing systemic health barriers.
About Black CAP
Since 1989, Black CAP has supported Black, African and Caribbean communities in Toronto affected by or at risk of HIV and STIs. As Canada’s largest Black-focused AIDS service organization, it provides culturally relevant prevention, outreach and support services. Facing stigma and systemic barriers, Black CAP relies on donors and volunteers to continue its work.
About APAA
Africans in Partnership Against AIDS (APAA), is a community-based, Canadian non-profit charitable AIDS service organization serving African communities in the greater Toronto area. Established in 1993, APAA has supported members of the African community in response to the increased need for those living with HIV/AIDS.
REACH Nexus Media Contact:
Andrew Russell
Senior Communications Specialist, REACH Nexus
andrew.russell@unityhealth.to
Phone: 416-268-7642
Frigid weather to persist and return, Environment Canada says
MAP director and scientist Dr. Stephen Hwang, spoke to CBC News about the health risk of frostbite during the recent cold snap. “Sometimes, people who are at risk don’t realize it because they’ve got to the point where their digits are becoming numb,” he told reporters. “So really, watching out for others who might be at risk and providing them with assistance is really important.”
Trump says ‘Housing First’ failed the homeless. Here’s what the evidence says
In this article from The New York Times, the author dives into the research surrounding the Housing First method, citing research lead by several MAP scientists and researchers. Using examples from Toronto, Massachusetts and California, this article looks at where Housing First shines and what the limitations are.
Why Canada needs a ready-to-run adaptive platform trial before the next pandemic hits
Op-ed by Dr. Benita Hosseini & Dr. Andrew Pinto for Healthy Debate
When the next pandemic arrives (and it will!) Canada will once again face urgent questions: Which treatments work? For whom? At what dose? And how quickly should we act?
During the COVID pandemic, we had to answer these questions without a reliable way to rapidly test outpatient treatments in community settings. Instead, we relied heavily on data from pharmaceutical-sponsored studies that often left significant ambiguity about how well a therapy would work in general populations. That uncertainty shaped billion-dollar procurement decisions and left health-care providers without clear guidance.
We now have an opportunity to change this.
A ready-to-run adaptive platform trial that stays in place to evaluate multiple treatments as soon as a threat emerges could ensure that Canada is no longer caught unprepared or dependent on evidence from elsewhere. This type of platform trial would be permanent, “always on” infrastructure to rapidly assess multiple treatments in real-world settings.
The Paxlovid story is a telling example. Canada purchased large quantities based on early trial data sponsored by the manufacturer. Those trials, while important, did not reflect the realities of outpatient care in Canada, where patients had different levels of vaccination, comorbidities and health-system access. It later became clear, only after additional data were released by the manufacturer, that the benefits were smaller than initially expected, especially for lower-risk groups.
This is not about criticizing any one trial. It is about recognizing that Canada had no mechanism to answer these questions for itself, quickly and independently. Without a rapid way to evaluate effectiveness in our own communities, governments had to make decisions with wide uncertainty and limited local data.
That vulnerability is still with us today.
Canada faces two structural challenges during health emergencies:
1- We do not have a rapid method to evaluate outpatient treatments. Most people with acute respiratory infections, whether COVID, flu, RSV or a future pathogen, are treated in primary care and emergency departments, not hospitals. Yet our research infrastructure has traditionally focused on acute care settings. This leaves us unable to quickly test therapies where they matter most.
2- We rebuild research infrastructure from scratch every time. Each new pandemic or emerging infection requires new teams, contracts, ethics approvals, data capture systems and protocols. This delays the start of trial by weeks or months; the exact period when governments are making critical decisions about what to purchase and how to deploy it.
The result?
Canada ends up making high-stakes clinical and procurement choices with limited local evidence. That is a fundamental vulnerability.
A ready-to-run platform trial can address this gap. The platform does not shut down between pandemics, it stays active, even at low intensity. When a new virus emerges or new therapy becomes available, enrolment can ramp up immediately, avoiding delays that come from reinventing the wheel.
It can test more than one treatment at a time. Instead of running separate trials, an adaptive platform can evaluate several therapies in parallel under one master protocol. This reduces cost, improves efficiency and accelerates decision making.
The adaptive platform evolves as evidence evolves; it allows ineffective treatments to be dropped and promising ones to be added. The trial adapts to changing variants, patient needs and scientific priorities.
Major international trials (such as RECOVERY and PANORAMIC in the United Kingdom and REMAP-CAP globally) showed how quickly adaptive platforms can produce reliable answers.
The next pandemic will not begin in hospitals. It will begin in walk-in clinics, family practices, urgent care centres and emergency departments. That is where clinicians see the earliest cases, and where early treatment decisions shape outcomes.
Evaluating treatments in these settings matters because:
1- Effectiveness varies based on timing of treatment and patient characteristics.
2- Many high-risk groups, including people facing economic insecurity, newcomers, and those without access to regular primary care, receive care in outpatient settings.
3- Early treatment can prevent hospital admissions and reduce pressure on emergency rooms.
Early steps are already underway. TreatResp (adapted from CanTreatCOVID, one of the largest outpatient trials conducted in Canada with 800 participants) offers an initial demonstration of how this model can work in community settings. But efforts like this will only reach their potential if they are treated as national infrastructure rather than short-term projects.
A standing trial embedded in community settings strengthens the entire system, not just hospitals. It also supports more responsible public spending. A standing platform would give decision-makers early signals about which drugs are effective, which groups benefit most and rapid data to support or revise guidelines.
In other words: better data, fewer costly mistakes.
There is growing recognition across health systems that preparedness cannot focus solely on stockpiles, vaccines or hospital surge plans. We also need the capacity to generate evidence, rapidly, locally and independently.
The window to build this is open today. Once the sense of urgency fades, it will be much harder to create sustained funding and political support. If we want to avoid repeating the uncertainty of the last pandemic, we need to act now.
Conflict of interest disclosure: Dr. Andrew Pinto is the Principal Investigator for CanTreatCOVID and TreatResp. Dr. Benita Hosseini is the co-Principal Investigator for CanTreatCOVID and TreatResp.
Did Toronto’s supervised consumption sites lead to more crime? Here’s what new research says
Dr. Mohammad Karamouzian spoke with the Toronto Star about crime rates surrounding supervised consumpton sites in Toronto. The study found that the sites have not led to a sustained increase in crime in the areas where they reside. In fact, in most cases, crime rates remained stable or even declined in the neighbourhoods they opened.
Upstream Lab scientists Drs. Archna Gupta & Saadia Sediqzadah awarded PSI Fellowships
Fellowships will support Dr. Gupta’s research into access to primary care and Dr. Sediqzadah’s research into youth with early phase psychosis
Dr. Archna Gupta and Dr. Saadia Sediqzadah, scientists at Upstream Lab (part of MAP Centre for Urban Health Solutions, St. Michael’s Hospital, Unity Health Toronto), have both been awarded 2026 PSI Graham Farquharson Knowledge Translation Fellowships.
The PSI Graham Farquharson Knowledge Translation Fellowship – valued at $300,000 per scientist for over two or three years – helps protect a promising new clinician-investigator’s research time, allowing the Fellow to undertake high-impact translational research in Ontario.
Knowledge translation research aims at transitioning research discoveries to the real world to improve health outcomes.
Dr. Gupta, a family physician and family medicine obstetrics provider at St. Michael’s Hospital, will use her fellowship for research into access to primary care in Ontario, at a key moment of transformation in the province’s health system.
“Ontario’s primary care system is facing major challenges, with many people struggling to find a family doctor or primary care clinician and access the care they need. The new Primary Care Act (2025) offers a unique opportunity to make meaningful improvements, setting out six patient-centred goals to increase access and strengthen care for all Ontarians. My research and knowledge translation activities are focused on helping Ontario’s primary care system evolve to meet these important targets,” says Dr. Gupta.
“This is a critical moment for health care in our province — a chance to make lasting, positive changes that will benefit every community. My research will play a key role in making care more equitable and accessible, informing policies and tools that support patients and health professionals alike. Ultimately, this research will help support a stronger, fairer primary care system — so that every Ontarian can get the care they need, when and where they need it most.”
Learn more about Dr. Gupta’s research into research into access to primary care:
- Understanding the relationship between the distance between patients and primary care providers and quality of care
- Primary Care Supply and Demand in Ontario
Dr. Sediqzadah, a psychiatrist at St. Michael’s Hospital, will use her fellowship for research to improve the mental and physical health outcomes for youth with early phase psychosis in Ontario. Her goals include developing the first patient decision aid for early phase psychosis that will be co-designed by people with lived experience (PWLE), their families/caregivers and healthcare providers.
“According to the Ontario Early Psychosis Intervention Program Standards, early phase psychosis (EPP) is defined as experiencing symptoms of a psychotic disorder between the ages of 14 and 35, who are either untreated or receiving treatment for 6 months or less. EPP can be a confusing time for a young person. The hallmark feature of psychosis is the difficulty in telling what is real and what is not. This often-persistent lack of insight has treatment implications for both the patient and their healthcare providers,” says Dr. Sediqzadah.
“Medication acceptance and adherence can be a challenge. The mainstay of treatment of psychotic illness includes antipsychotics. While effective, they carry a significant burden of metabolic syndrome, including weight gain and increased risk of diabetes. Concerns about the side effects, how long one must be on medication, or even simply accepting one has a mental illness that requires medication in the first place, can be common concerns and barriers to treatment. We lack tools to address these issues that are tailored to both prescribers and patients, especially those that include people with lived experience in the development process. As such, my proposed research will employ knowledge translation approaches to guide both patients and prescribers on psychosis treatment, as well as the prevention/management of metabolic side effects of antipsychotics.”
Learn more about Dr. Sediqzadah’s research into youth with early phase psychosis:
- Reasons for Hope: “When can I stop taking it?”: Early phase psychosis patient decision aid co-designed by patients, families and providers
- Metformin, Antipsychotics and Psychotic Disorders: Challenges and Opportunities in Family Medicine and Psychiatry
For more information or to request an interview with Dr. Gupta or Dr. Sediqzadah, please contact: upstreamlab.comms@unityhealth.to
Alberta syphilis cases fell after rapid testing rollout, study co-led by St. Michael’s finds
Dr. Sean B. Rourke, a scientist with MAP Centre for Urban Health Solutions (left) and Dr. Ameeta Singh, an infectious disease specialist at the University of Alberta (right)
A new study suggests that syphilis cases in Alberta dropped sharply following the expansion of rapid testing and same-day treatment, reversing years of steep increases and growing concerns about congenital transmission.
The study, co-led by researchers with MAP at St. Michael’s Hospital, University of Alberta, and Indigenous Services Canada, was conducted as Alberta declared a syphilis outbreak in July 2019 after cases surged among key populations, especially Indigenous communities.
In Alberta, the scale of the crisis was stark: reported syphilis cases jumped from 161 in 2014 to 2,330 in 2019. Between 2015 and March 2024, there were 350 cases of congenital syphilis – where syphilis is passed from mother to child – resulting in 61 stillbirths.
To help reduce transmission, Dr. Ameeta Singh, an infectious disease specialist at the University of Alberta, and her team introduced rapid, point-of-care syphilis testing. This approach allows people to be tested and treated in a single visit, often in community-based or non-traditional settings. A key factor in its success was the use of mobile health teams who reached individuals with limited access to care, providing testing and connecting them to treatment in culturally safe ways.
The province first implemented the rapid point-of-care testing program in Edmonton in August 2020 and expanded across Alberta in March 2022. Researchers used interrupted time-series analyses to evaluate how the rollout affected new syphilis positivity rates, comparing trends before and after the intervention to measure its impact. After the Edmonton rollout, monthly rates dropped by 15 percent, and once the program expanded across Alberta, the decline deepened to 25 percent, the study found.
“Rapid testing didn’t just slow the outbreak, it bent the curve and now the number of new infections is declining,” said Dr. Ameeta Singh, an infectious disease specialist at the University of Alberta. “Expanding these tests, in addition to offering treatment and care, has helped us reach people in remote or underserved communities who are too often missed by traditional healthcare systems.”
Overall, the findings show that introducing rapid syphilis testing was associated with a meaningful reduction in new infections in a high-income setting facing renewed heterosexual transmission and persistent barriers to testing and timely treatment.
“Infectious syphilis is a public health emergency in Canada, hitting communities in Alberta, Saskatchewan and Manitoba the hardest,” said Dr. Sean Rourke, director of REACH Nexus at the MAP Centre for Urban Health Solutions at St. Michael’s Hospital (Unity Health Toronto). “This data show that we can make a real-world impact by reaching more people to test, diagnose, and create crucial linkages to care to help end this health crisis.”
“Our work highlights the importance of having the right healthcare teams in place to engage and support people who face barriers to care, including stigma, discrimination, and racism,” he said.
This study, along with several others, helped contribute to Health Canada’s approval of a dual HIV/Syphilis in 2024 and standalone syphilis test in 2025.
Health officials say the findings highlight the need for accessible, low-barrier testing, as key populations across Canada—particularly Indigenous and remote communities—continue to face disproportionately high rates of syphilis and other sexually transmitted and blood-borne infections.
“Rapid syphilis testing is an important part of delivering culturally safe, trauma-informed care for First Nations, Inuit, and Métis communities,” said Dr. Tom Wong, Chief Medical Officer of Public Health at Indigenous Services Canada. We will continue working closely with partners and community leaders to strengthen community-led solutions and create spaces that support healing and well-being.”
By Andrew Russell for Unity Health Toronto