MAP Scientist Dr. Tara Kiran spoke to the New York Times for a story on Canada’s primary care system and efforts being taken to attract more family doctors, particularly in rural areas.
Author: Emily Holton
Director’s update: MAP’s 2025 in review
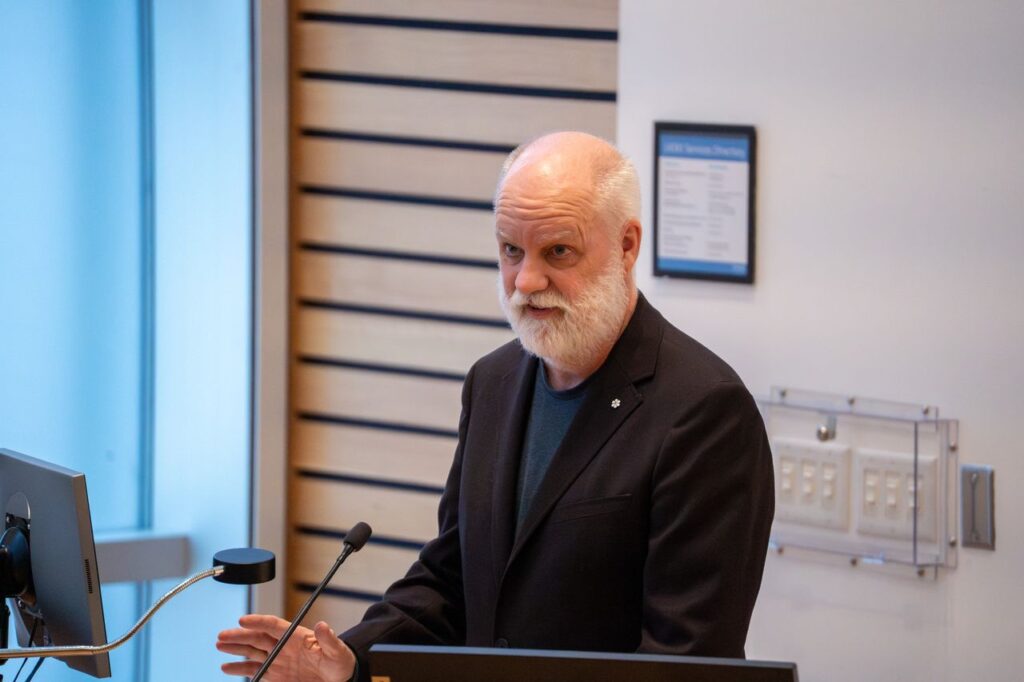
Pictured above, from left to right: MAP Director Dr. Stephen Hwang and MAP scientist Dr. Tara Kiran at the 2025 MAP Solutions for Healthy Cities Symposium, in discussion with Dr. Andrea Tricco (Executive Director Li Ka Shing Knowledge Institute), Stephen Lucas (former Deputy Minister of Health Canada) and Dr. Fahad Razak (Li Ka Shing Scientist).
Message from MAP Director Dr. Stephen Hwang

With 2026 on the horizon, I’m incredibly proud to share some of MAP’s successes from the past 12 months. Some highlights (click here to jump to the full report):
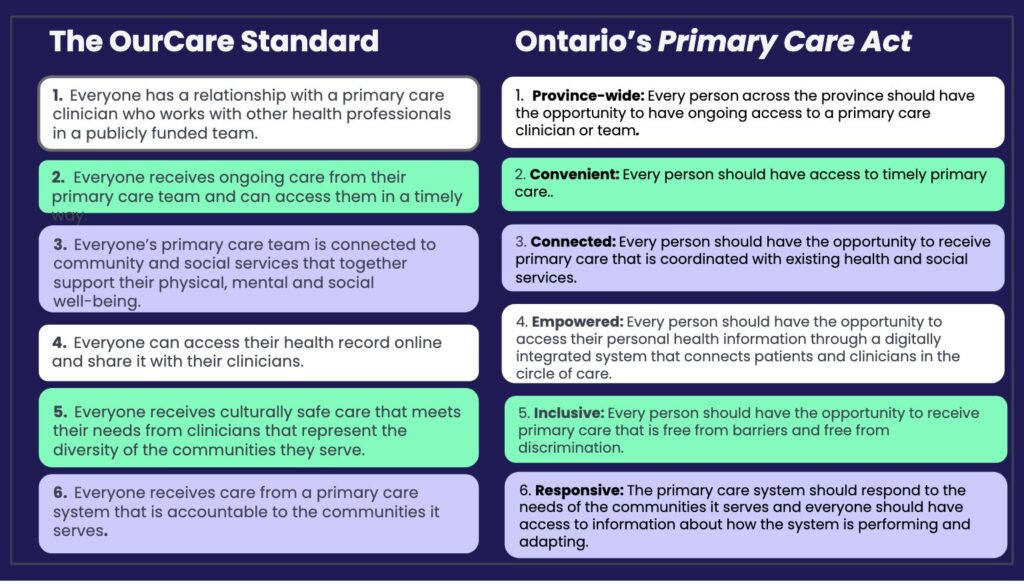
- In Ontario, a new Primary Care Act mirrors MAP’s OurCare Standard, setting ambitious, patient‑centred goals for the province’s health system.
- Nationally, Canada’s first National School Food Program was made permanent in 2025, providing meals to 400,000 children and saving families hundreds of dollars annually.
- Thanks to recent Our Healthbox launches in the Northwest Territories, MAP’s programmatic reach now officially stretches from coast to coast to coast.
- MAP was spotlighted in more than 100 media features and published more than 250 peer-reviewed papers, leading and defining the conversation on what a healthier Canada can look like.
Through each of the stories above and below, I see MAP’s core values in action: world-class research to strengthen Canada’s policies and practices; community partnerships to bring evidence-based health innovations to the places they’re needed most; and a deep commitment to put equity and respect for lived expertise at the centre of everything we do.
These stories also underscore the importance of persistence. Many of this year’s wins were years in the making.
On behalf of MAP’s leadership, researchers, staff and students: thank you to MAP’s many community, academic and policy partners and to MAP’s visionary donors and funders.
Step by step, we are charting the course toward a healthier, safer and more inclusive Canada. Our successes are only thanks to your partnership and commitment. We are grateful to do this work with you.
Sincerely,
Dr. Stephen Hwang
Director, MAP Centre for Urban Health Solutions
Canada Research Chair in Homelessness, Housing and Health
2025 Research Highlights

Canada’s first National School Food Program: Permanent federal funding, local implementation: In 2024, MAP’s Dr. Katerina Maximova helped develop Canada’s first-ever National School Food Program. In 2025, Prime Minister Carney announced that the federal government is making the national program permanent. At the local level this year, Dr. Maximova served on Toronto’s Universal Student Food Program Steering Committee which developed the city’s vision and strategy for universal school meals. City Council unanimously adopted the plan in June. The city will now provide a morning meal in all Toronto school communities by the 2026/27 school year and introduce a lunch program by 2030.

Historic primary care act based on MAP recommendations: In June, the Ontario government introduced the Primary Care Act, a framework of six ambitious, patient-centred objectives for Ontario’s primary care system. The framework is an almost word-for-word reflection of MAP’s OurCare Standard. Watch here as OurCare lead Dr. Tara Kiran reflects on what this means for patients. Dr. Kiran just wrapped up a second phase of the OurCare study (learn more: The Globe and Mail, Toronto Star) and continues to champion implementation of the OurCare Standard nationwide.

MAP reaches the far north, distributes lifesaving supplies across Canada: Since MAP’s first Our Healthbox smart vending machines launched in 2023, MAP has now distributed almost 2,000 free HIV self-tests, more than 37,000 harm reduction supplies and almost 4,000 Naloxone kits — reaching 15,700 people in 22 communities across Canada. In 2025, the program continued to expand with new Healthboxes in New Brunswick (Miramichi), Ontario (Toronto, North Bay), Manitoba (Winnipeg), Alberta (Piikani Nation) and the Northwest Territories (Behchokǫ̀, Hay River, Inuvik and Yellowknife).

MAP drug checking initiative receives $3M of new federal funding, protects thousands across Ontario: In 2023, MAP received $2M of federal funding to create Ontario’s Drug Checking Community, an expansion of MAP’s public health and safety program, Toronto’s Drug Checking Service. This October, Health Canada committed an additional $3M to the program with the goal of establishing a collection site in each of Ontario’s 29 public health unit jurisdictions by December 2027. The service prevents overdose and saves lives every day by rapidly analyzing tiny drug samples to detect and describe unexpected — and often lethal — ingredients. Results not only inform people who use drugs, but also equip community health workers, public health units, first responders, policy makers and others with vital intelligence about what’s circulating in the unregulated drug supply. Since Toronto’s Drug Checking Service launched in 2019, the program has now checked more than 20,000 samples of drugs and used drug equipment.

MAP’s national partnership with Staples Canada reaches 5-year milestone: Launched in early 2021, Even the Odds is a partnership between Staples and MAP to raise awareness of inequity in Canada and to help create vibrant, healthy communities. Through corporate donations and fundraising, Even the Odds funds MAP research and innovative, evidence-based solutions across Canada — to help make the future fair for everyone. Originally struck as a five-year, $5M commitment, we are thrilled to share that the initiative has now raised more than $8M and will continue through a new, multi-year agreement. MAP is incredibly grateful for Staples’ unwavering vision, commitment and transformative support.

First phase of pharmacare comes to life in BC, Manitoba, PEI and the Yukon: In 2024, Canada passed a new pharmacare law that was strongly influenced by MAP research. In 2025 BC, Manitoba, PEI and the Yukon were the first jurisdictions to sign federal Pharmacare agreements, and will now provide residents with free coverage for contraceptives and some diabetes medications. In November, a federal committee chaired by MAP’s Dr. Nav Persaud published its recommendations for launching and paying for a fully single-payer pharmacare program across the country.

MAP’s Navigator program opens third site in Montreal, reaches 1,000 patients: MAP’s signature Navigator Program pairs hospital patients who are homeless with an outreach counsellor — a ‘Navigator.’ The Navigator gets to know the patient and connects them with the health and social support they need to break cycles of homelessness and poor health, and to move forward in securing housing that works for them. Thanks to Even the Odds (Staples Canada), MAP expanded the program to St. Paul’s Hospital (Vancouver) in 2023 as well as Centre hospitalier de l’Université de Montréal (CHUM) in 2025. This summer, Navigator reached a major milestone: the national program served its 1,000th patient (learn more: CTV Your Morning, CBC).

A new standard for violence prevention and survivor-centred care: The first program of its kind in Canada, MAP’s Safe at Home program has now empowered 52 women and gender-diverse people to end violent situations at home — without facing displacement. Delivered in partnership with Mission Services of Hamilton, this innovative model requires the perpetrator of violence to leave the family home. Survivors and their children have the option to safely remain in place, protected by Safe at Home’s integrated supports from health, social, police and legal services. MAP is now building new partnerships to expand the program and help more people to access safety, stability and support where they live.

MAP initiative identifies hundreds of undiagnosed HIV and syphilis infections, connects to culturally safe care: In March, MAP launched the Ayaangwaamiziwin Centre — a groundbreaking public health response to the alarming rise in HIV and syphilis rates in the Prairies and northern territories. The Centre has already reached and tested more than 2,000 people across Alberta, Saskatchewan and Manitoba, identifying more than 200 previously undiagnosed cases of HIV and syphilis and connecting patients to culturally safe treatment and preventative care. Named after the Ojibwe word for ‘carefulness and preparedness,’ the Ayaangwaamiziwin Centre will soon expand to new sites in the Northwest Territories, Yukon and Nunavut.

MAP rewrites Canadian clinical guidelines for HIV prevention medication: MAP scientist Dr. Darrell Tan led a major update to Canada’s HIV prevention medication guidelines, published in December in the Canadian Medical Association Journal. The new guidelines centre equity and access, and offer Canadian healthcare providers and policy makers the latest insights on how to ensure lifesaving HIV medications are effectively prescribed. A key change: providers are now advised to prescribe PrEP to anyone who requests it — even if patients choose not to disclose HIV risk factors. This shift in practice would remove barriers created by clinician ‘gatekeeping’ and recognizes the realities of stigma and discrimination. Marginalized communities continue to face disproportionately higher barriers to HIV prevention and care.


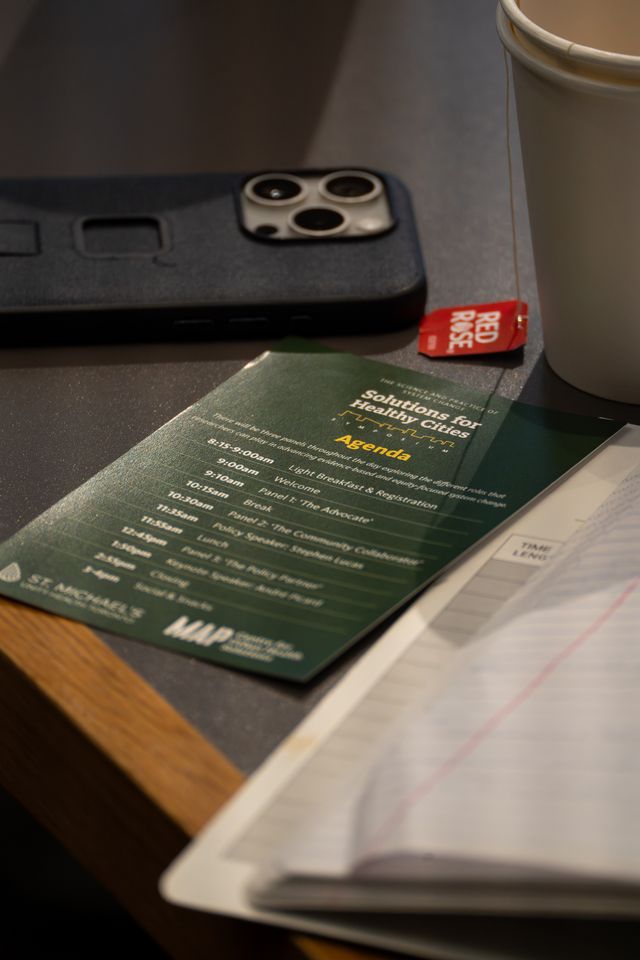
MAP hosts 2025 Solutions for Healthy Cities Symposium: On November 25, almost 200 researchers, service providers, policymakers, students and community experts gathered at St. Michael’s Hospital in Toronto to explore and discuss a multifaceted challenge: how to advance evidence-driven and equity-focused system change in Canada. The 2025 Solutions for Healthy Cities Symposium comprised a full day of talks, discussion and Q&As with policy-focused researchers and insightful guest speakers — including keynote André Picard, one of Canada’s top health and public policy observers and commentators.

MAP x APPLE Schools: Healthier futures for 4,500 more kids in 2025: APPLE Schools is an internationally recognized best practice that has been proven to help kids move more, eat better and feel happier – erasing many of the long-term health effects of childhood poverty. MAP’s implementation and evaluation of the award-winning program continues in 17 elementary schools in disadvantaged Ontario and Alberta neighbourhoods, with plans to expand to reach more students in 2026. What does it look like to be an APPLE School? Here’s an adorable moment with a grade one student, and an example of an APPLE Schools activity that builds movement into the school day.
Primary Focus reaches Top 5 in Apple’s Medicine podcasts, wins international award: Launched in February, MAP scientist Dr. Tara Kiran’s Primary Focus podcast has already gained an active audience in 22 countries, won an eHealthcare Leadership Award and reached the Top 5 in Apple’s Medicine podcast charts. It’s also a finalist for the Canadian Online Publishing Awards in the Best Podcast category. Now in its second season, the podcast brings together the voices of frontline healthcare workers, patients, researchers and policymakers to unpack the issues and innovations that could — and should — transform primary care in Canada.
MAP’s awards and recognition continue to grow: Two out of the three prestigious CIHR Institute of Population and Public Health Trailblazer Awards were awarded to MAP scientists in 2025, recognizing their exceptional contributions to public health research. MAP is also now home to seven Canadian Academy of Health Sciences (CAHS) Fellows (+1 in 2025) and three Government of Canada King Charles III Coronation Medal award winners (+2 in 2025). This year, MAP researchers were awarded the inaugural Royal Society of Canada Eric Jackman Prize, a 2025 Vanier Canada Doctoral Award (Canadian Institutes of Health Research) and two PSI Graham Farquharson Knowledge Translation Fellowships. From the University of Toronto, MAP researchers won the 2025 Peggy Leatt Knowledge & Impact Award (Institute of Health Policy, Management and Evaluation), Louise Lemieux-Charles Health System Leadership Award (Institute of Health Policy, Management and Evaluation), 2025 Doctoral Award (Emerging and Pandemic Infections Consortium/EPIC), Excellence in Research: Mid Career Researcher Award (Department of Family and Community Medicine), Faculty Recognition Award for Exceptional Mentorship — (Institute of Medical Science) and the Dean’s Alumni Award (Temerty Faculty of Medicine). Finally, a MAP collaboration with The Local Magazine won the Jackman Award for Excellence in Journalism at the 2025 Canadian Journalism Foundation Awards.
Want more research updates?
Follow us on LinkedIn and subscribe to MAP’s Junction e-newsletter for short, monthly updates on our studies, our solutions and the issues we study.
MAP hosts 2025 Solutions for Healthy Cities Symposium
On November 25, 2025, almost 200 researchers, service providers, policymakers, students and community experts gathered at St. Michael’s Hospital in Toronto to explore and discuss a multifaceted challenge: how to advance evidence-driven and equity-focused system change in Canada.
The symposium comprised a full day of talks, discussion and Q&As with policy-focused researchers and insightful guest speakers. This was the third Solutions for Healthy Cities Symposium hosted by MAP, and the first that MAP co-hosted with the St. Michael’s Hospital Urban and Community Health Research Pillar.
About the 2025 Symposium

For many public health and population health researchers, the ultimate goal is to enable system change—to improve health and well-being, and to empower everyone to live with dignity. We believe that Canada’s health and social policies should be grounded in the best possible evidence, and we want to help make that happen.
In practice, what can that process look like? At a time when science itself is politicized, what are the roles researchers can play in enabling and advancing evidence-based and equity-focused policymaking and policy implementation in Canada?
Participants joined us to explore these questions, hear from insightful guest speakers and discuss how researchers and policymakers can be more successful in advancing equity-focused system change.
Keynote: Andre Picard

André Picard is one of Canada’s top health and public policy observers and commentators. He is the health columnist at The Globe and Mail, where he has been a staff writer for more than 30 years. He is also the author of numerous books and has received much acclaim for his writing and for his dedication to improving healthcare, including earning him the National Newspaper Award as Canada’s top newspaper columnist.
Speakers

Panels explored the different roles that research and researchers can play in advancing evidence-based and equity-focused system change: ‘the advocate,’ ‘the community collaborator’ and ‘the policy partner.’
Panel 1: ‘The Advocate’

Najma Ahmed is a trauma surgeon, Interim Executive Vice President and Chief Medical Officer at Unity Health Toronto. In 2019 she formed Canadian Doctors for Protection from Guns to address gun violence as a public health issue, and played a key role in advancing Canada’s 2020 assault weapons ban. The group now has nearly a thousand members across the country. Read more

Mikaela Gabriel is a clinical and counselling psychologist, Canada Research Chair in Indigenous Women and Two-Spirit Mental Health and Homelessness and a scientist at both MAP Centre for Urban Health Solutions and Well Living House. Her research explores Indigenous health and wellbeing, urban cultural connection and housing transitions for Indigenous Peoples in Canada. Read more

Mina Tadrous is an ICES scientist, Canada Research Chair in Pharmaceutical Policy and Real-world Evidence and co-director of Pharmaceutical Policy and Pharmacy Practice at the Ontario Drug Policy Research Network. His research focuses on evaluating drug policies and working closely with policymakers on drug safety and effectiveness. Read more

Nav Persaud is a family doctor, Canada Research Chair in Health Justice, scientist at MAP Centre for Urban Health Solutions and chair of the the Government of Canada’s Committee of Experts to make recommendations on National Pharmacare. Dr. Persaud’s research is dedicated to narrowing the health gap between the highest and lowest wealth brackets, and to ensuring that everyone in Canada can afford the food and medication that they need. Read more

Seema Marwaha (moderator) is the Editor-in-Chief of Healthy Debate (healthydebate.ca), where she brings years of experience in journalism, advocacy and health communication. She is also an internal medicine physician at St. Michael’s Hospital and an investigator with the St. Michael’s Hospital Urban and Community Health Pillar. She is the current president elect of the Federation of Medical Women of Canada and a regular contributor to various Canadian media publications. Read more
Panel 2: ‘The Community Collaborator’

Sacha Bragg is an Opioid Research Communication and Project Liaison with Chiefs of Ontario. She has also been a researcher with the Thunderbird Partnership Foundation, championing culturally-based addictions, substance use and mental wellness services for First Nations in Canada. Learn more

Diana Chan McNally is a community and crisis worker in Toronto’s downtown east side, founder and coordinator of the Ontario Coalition for the Rights of Homeless People, and an instructor in George Brown College’s Community Worker program. As someone with lived experience of social services and of being unhoused, Diana’s work focuses on human rights and equity issues for people who are experiencing homelessness by advocating at the political level, while still maintaining an active frontline praxis. Read more

Zoë Dodd is MAP’s inaugural Community Scholar. She has worked in harm reduction for almost 20 years as a program coordinator, organizer and advocate. She helped develop a model of treatment and support for people who use substances living with Hep C, which has been adopted in several areas across Ontario. Read more

Mohammad Karamouzian is an infectious disease epidemiologist and scientist with the Centre on Drug Policy Evaluation, based at MAP Centre for Urban Health Solutions. He is also affiliated with the BC Centre on Substance Use and the WHO Collaborating Centre for HIV Surveillance in the Middle East and North Africa. His research focuses on addressing health inequities faced by marginalized populations such as female sex workers, people who inject drugs and those who are incarcerated, and on translating his findings into policy. Learn more

Tara Gomes (moderator) is a professor at the University of Toronto, Canada Research Chair in Drug Policy Research and Substance Use, Scientific Director of the St. Michael’s Urban and Community Health Research Pillar, scientist at MAP Centre for Urban Health Solutions and the principal investigator of the Ontario Drug Policy Research Network. Through her research, she is working to develop evidence, tools and best practices to strengthen drug policy decision-making in Canada and around the world. Read more
Panel 3: ‘The Policy Partner’

Stephen Hwang is an internal medicine physician, Canada Research Chair in Homelessness, Housing and Health and director of MAP Centre for Urban Health Solutions. His success co-leading the At Home/Chez Soi study persuaded the federal government to commit to scaling up Housing First interventions across Canada. Read more

Tara Kiran is a family doctor, scientist at MAP Centre for Urban Health Solutions and the Fidani Chair in Improvement and Innovation at the University of Toronto. Her OurCare study was Canada’s largest-ever public engagement on primary care reform, and provided the blueprint for Ontario’s 2025 Primary Care Act. Read more

Stephen Lucas is the CEO of Mitacs, science policy advisor to Unity Health Toronto and former Deputy Minister of Health Canada. He brings four decades of public sector experience in economic, innovation, energy, environment, health and social policy development. Read more

Fahad Razak is an internal medicine physician, Canada Research Chair in Healthcare Data and Analytics and a scientist with the St. Michael’s Urban and Community Health Research Pillar. He served as the Scientific Director of the Ontario COVID-19 Science Advisory Table, shaping the province’s pandemic response. Read more

Andrea Tricco (moderator) is the Executive Director of the Li Ka Shing Knowledge Institute at St. Michael’s Hospital and a scientist in the Knowledge Translation Program. She is a professor in the Dalla Lana School of Public Health, University of Toronto and holds a Tier 1 Canada Research Chair in Knowledge Synthesis. She is Co-Editor in Chief of the Journal of Clinical Epidemiology. Her research focus is on advancing the science of knowledge synthesis and responding to the needs of decision-makers (including policy-makers, healthcare providers and patients) through knowledge synthesis. Read more
Learn about MAP’s past symposiums

2023: The science and practice of implementation success
On March 23, 2023, almost 200 researchers, service providers, policymakers, students and community experts gathered at the second Solutions for Healthy Cities Symposium to explore our 2023 theme: The science and practice of implementation success. Keynote speaker Dr. Ibram X. Kendi joined the event virtually, in conversation with MAP Director Dr. Stephen Hwang and followed by a Q&A with the audience. Learn more

2020: Co-designing for real world impact
At the first Solutions for Healthy Cities Symposium on March 2-3, 2020, MAP Centre for Urban Health Solutions launched 10 collaborative solutions networks with a common goal: to effect real-world social change by co-designing and demonstrating what works to address critical urban health challenges in our communities. The symposium gathered more than 170 network members including scientists, community partners, policy makers, and people with lived expertise from across the country. Learn more
Thank You
This symposium was made possible thanks to Even the Odds (a partnership of MAP and Staples Canada), the St. Michael’s Foundation and the generous contributions of our visionary donors.
MAP policy impact: Federal government makes National School Food Program permanent

On October 10, 2025, Prime Minister Carney announced that the federal government is making the National School Food Program permanent. The program provides meals for up to 400,000 children in Canada and aims to save families with two children $800 per year on groceries.
Canada was previously the only G7 country with no national school food program. First announced in Budget 2024 with an investment of $1 billion over five years (2025-29), the National School Food Program will now receive permanent funding of $216.6 million per year starting in 2029/30. The Government of Canada has signed bilateral agreements with all provinces and territories to continue implementation and expansion of the program.
MAP’s contribution: In Fall 2022, MAP Scientist Dr. Katerina Maximova was part of the national opening roundtable to shape the new pan-Canadian School Food Policy. Dr. Maximova’s role was to provide a research perspective and help ensure that the policy is grounded in the best available evidence.
“This funding is already improving the lives of many thousands of children in Canada,” said Dr. Maximova. “To make it permanent was always the goal. It’s a very exciting day.”
In January 2025, Dr. Maximova also advised the City of Toronto on implementation of the federal funding, through their Universal Student Food Program Steering Committee. The City subsequently committed to providing a morning meal in all Toronto school communities by the 2026/2027 school year and to introduce a lunch program by 2030.
Our impact so far: MAP’s Navigator program in downtown Vancouver
Oct. 10, 2025
MAP’s Navigator program pairs hospital patients who are homeless with an outreach counsellor – a ‘Navigator’ – who gets to know the patient and helps them plan for discharge.
Where will the patient live after they leave the hospital? How will they manage medications, and get to follow-up appointments?
These questions can be complex, but the Navigator walks alongside the patient to sort through the answers – both while they’re in hospital and in the months following. The goals are to better support unhoused patients as they recover from hospitalization, connect them with healthcare and social services in the community, and ultimately, to help people exit homelessness for good.
MAP designed and launched the Navigator Program as a St. Michael’s Hospital pilot in 2019. As the program grew, the positive impact on St. Michael’s patients – and their care teams – was clear. That’s why MAP and Staples Canada, through our Even the Odds partnership, expanded Navigator to St. Paul’s Hospital (Vancouver) in 2023 followed by Centre hospitalier de l’Université de Montréal (CHUM) in 2025.
Across all sites, the Navigator program has now served more than 1,000 patients.
To mark World Homeless Day on Oct. 10, we talked with Dr. Anita Palepu at St. Paul’s about the program’s impact so far.

“When MAP and Staples approached us to see if Navigator might be feasible at St. Paul’s, it was clear that the program was a perfect fit. We serve many people who are vulnerably housed or homeless, many of whom have complex medical issues. We were experiencing all the same challenges that St. Michael’s had experienced.
Hospitals are always working at full capacity. When people don’t need acute hospital care anymore, we must discharge them to make the bed available for people who are sicker. But for our unhoused patients, that often meant we had to send people straight from the hospital to a shelter, or even to the street because the shelters were full. It was a huge gap in care, and often people ended up right back in hospital. It’s a really difficult cycle to break.
The support from Even the Odds meant we could hire Alex, our new ‘Navigator’, in this very specific role. MAP supported us in designing and adapting the program for our hospital. We went for site visits and got to know how the program worked in Toronto. We are still in close contact, sharing our learnings back and forth. Our whole team – our program directors, nurses, social workers, and all our allied team – have all been extremely enthusiastic, because we all saw the need, and now we are seeing the successes as well.
Just like at St. Michael’s, our unhoused patients are both medically and socially complex. Many are living with a really challenging combination of poverty, isolation, serious mental health disorders and substance use. Without shelter and support, people age rapidly, and die early.
I wish we could solve the more structural issues in our society that would prevent this from happening to people. But thanks to Staples, MAP and the Navigator program, we can now care for them the best we can, with all the levers we have access to.
We are incredibly grateful for Staples’ generosity and ongoing support. It means a lot that they believed in the program and wanted to see it expand. It’s all been a really wonderful experience for St. Paul’s.”
MAP policy impact: Ontario Primary Care Act, 2025

On June 5, 2025, the Government of Ontario passed the Primary Care Act, a framework of six ambitious, patient-centred objectives for Ontario’s publicly funded primary care system.
The objectives are clearly based on MAP’s OurCare Standard—six statements that describe what every person in Canada should expect from our primary care system.
“To call this historic is an understatement,” said MAP scientist, OurCare lead and U of T Fidani Chair Dr. Tara Kiran.
This legislation will make Ontario the first Canadian jurisdiction to establish a framework to improve its primary care system. The Minister is now required to prepare an annual report describing how the Government of Ontario is working to achieve the Act’s objectives.
About OurCare: In 2023, MAP led the largest-ever public consultation on primary health care, collecting input and ideas from close to 10,000 people across Canada. In 2024, we distilled what we heard into the groundbreaking OurCare Standard: six simple statements that describe what every patient in Canada should be able to expect from primary care. The Standard represents a concrete and achievable vision and a new benchmark for assessing the quality of primary care in Canada. This national initiative was made possible through generous support from Staples Canada (Even the Odds), Max Bell Foundation and Health Canada.

Voices of impact: Celebrating Black excellence, leadership and joy at MAP


In celebration of Black History Month, Denese Frans-Joseph (MAP Research Equity Specialist) and Christina Salmon (MAP Senior Manager of Research Programs and Partnerships) sat down with Wale Ajiboye, Jolen Kayseas and Martha Taylor to talk about their inspirations, their work at MAP and their advice for the next generation of Black researchers and health equity leaders.

Martha Taylor (she/her) is the coordinator for the MAP Summer Student Program and co-leads MAP’s Anti-Racism and Equity Advisory (AREA) group. She is an African woman who graduated from Trinity College at the University of Toronto with an Honours Bachelor of Arts in Health Studies, German and Portuguese. She has a deep passion for racial (health) equity work and working with communities. Her goal is to become a doctor.

Jolen Kayseas (he/him) is an Afro-Indigenous Research Coordinator at MAP. He has contributed to research initiatives addressing health outcomes for marginalized people, including people who use drugs and people experiencing homelessness, and has contributed to developing actionable program recommendations. Jolen is currently volunteering in Accra, Ghana, working on a project focused on educational outcomes and sustainable learning environments.

Dr. Wale Ajiboye (he/him) is a senior research associate and adjunct scientist at MAP. Wale’s research seeks to understand the behavioral, biomedical, social and structural determinants of HIV vulnerabilities; and to develop, adapt, test, implement and scale-up strategies to reduce the rates of HIV infection in Black communities in Canada and the Global South.
Denese Frans-Joseph: Thank you so much for joining us today. To start, I would love to hear from all three of you about what inspired you to pursue a career in urban health research. How does your work contribute to advancing health equity?

Martha Taylor: I came to Canada as a child refugee at the age of seven, which ultimately laid the foundation for my interest in urban health research. I watched my parents struggle to navigate the Canadian healthcare system, but it wasn’t until I got older that I came to understand how my family’s experience wasn’t unique, but was rather the result of a settler society built on anti-Black and anti-Indigenous racism. As a result, I’ve always gravitated towards work and volunteer opportunities that challenge racial health inequities. Currently at MAP, my work contributes to advancing racial health equity in two ways. As the co-lead for MAP’s Anti-Racism and Equity Advisory group, called AREA, working with my wonderful co-lead Denese and our AREA members ensures I help to inform how racial equity is incorporated into MAP’s strategic goals, policies and practices. And as the coordinator for the MAP Summer Student Program, I work with our Summer Student Working Group to ensure that Black, Indigenous and racialized undergraduate students have the opportunity to experience research in a safe and supportive environment. I think this is particularly important because traditional research environments lack representation, so I’m happy to be in a position where I can inspire students to see and know that research doesn’t have a colour.

Jolen Kayseas: When I started my undergrad in 2018 at TMU, I didn’t know what I wanted to go to school for. I just knew that I wanted to learn, read as much as I can, and understand the world as a new adult. I started in linguistics and as an ethnography researcher. And then in my second year, COVID hit. We all saw how it affected everyone, but especially us Black people, and the disparities that Black people face compared to non-Black people. I’ve always been into social justice, equity and asking, ‘Why? Why are things like this? Why are there disadvantages for certain identities?’ That’s when I knew I wanted to do something within the social determinants of health. So I reached out to the Indigenous Office at TMU and asked if there are any opportunities to work or volunteer, in any capacity, in this area. And lo and behold, MAP’s first, pilot Summer Student Program was starting soon, and they encouraged me to apply. I applied, and I started on Stephen Hwang‘s team, working with Jesse Jenkinson on a project called Ku-gaa-gii pimitizi-win: Vaccine uptake, confidence and hesitancy among people experiencing homelessness in Toronto. It was that summer that I really knew that I wanted to work in urban health research and continue asking why, and pushing back against people saying, ‘Oh, this is just how it is.’ I’m here still, four years later, and I’ve loved every project I’ve been a part of. I’ve learned so much from everybody that I’ve come across, whether that be in community expert groups, interviewing folks, working alongside people, or going to events at St. Michael’s Hospital. I hope to continue working in urban health research as long as I can.

Wale Ajiboye: My background is in pharmacy, and I worked as a clinical pharmacist for several years taking care of different types of patients, including those with advanced AIDS. It was very painful to see people go through a lot when there are effective medications that can be used to treat and to prevent HIV infection. I didn’t have a lot of experience with HIV prevention, but I felt that I could do more to address HIV-related disparities in Black communities and in Black people generally, by focusing on HIV prevention rather than waiting to do clinical treatment for those that already have the infection. After I got my PhD and relocated to Canada, I felt this would be a good opportunity for me to be involved in urban health rather than clinical work. I was fortunate to meet Dr. LaRon Nelson, and realized that the work he was doing aligned with my interest. I was really, really excited, because it was a perfect opportunity for me. Even though I started as a volunteer and worked for almost one year as a volunteer, I did it passionately because it was something that I really love to do: preventing HIV infection through the use of PrEP, a medication for preventing HIV infection. Since then, our work has helped to promote equity by reducing HIV-related disparities, because our work is focused on designing and implementing strategies that can increase the access, uptake and use of HIV prevention tools.
Christina Salmon: Could you share a project or research initiative at MAP that you’re particularly proud of, and its impact on the communities you serve?

Martha Taylor: Without a doubt, I’m proud of the MAP Summer Student Program and our collaboration with the Community of Support – Research Application Support Initiative. Sixty-six per cent of the students that participated in last year’s program are Black which was absolutely marvelous, since it exemplified the importance of intentional collaborations and initiatives that target communities that are historically underserved. I’ll never forget the happiness I felt after our most recent research rounds. One of our students told a member of her team that our program showed her that research didn’t have a face. I believe this demonstrates MAP’s commitment to increasing representation and I hope this program is one that continues to grow and flourish.

Jolen Kayseas: I’ve worked on a few projects, but one that really, was really amazing to be a part of was called People experiencing marginalization and the effects of the COVID-19 pandemic response (MARCO). That project had so many different parts to it, but the question that I worked on was, how were issues of racism addressed during the COVID-19 pandemic? I worked alongside Michelle Firestone, who is a great ally and advocate of the Black community. It was really interesting because the data was being collected in the summer of 2021 when George Floyd was murdered and Black Lives Matter was at the forefront. This particular study was an amazing experience, because Michelle really let me drive the research and the writing, and help with the analysis to make sure that was impactful. We found that within that research, in the data that we collected, a lot of institutions were confronting anti-Black racism, but they weren’t really understanding how their policies might directly and indirectly contribute to racism that both employees and patients experience. A lot of organizations also leaned on their employees to deal with institutional racism. I’m very proud of that study and the work that we did.

Wale Ajiboye: I led the adaptation and pilot implementation of an intervention, Culturally Responsive HIV Prevention Services for Black Communities in Canada. The goal is to develop the capacity of HIV prevention providers on how to provide culturally competent services. Upon piloting the intervention, we heard from healthcare providers that we helped them identify some of their practices that they did not know were actually in conflict with the culture of Black people. I’ll give an example. One of the providers mentioned that when you are late for an appointment, 15 minutes late, then you are not going to have access to your provider. But through the capacity building, they realized that there are many structural barriers that Black people face in accessing health care, and structuring their appointment system that way is very problematic. They realized it’s better for them to leave it open, to remove that barrier. After eight months, we did a post-intervention survey, and they told us that making those adjustments really helped to be able to increase the number of Black folks that were retained in their care. So that was an interesting initiative, I think that’s something that I am really proud of. I’m currently partnering with OHTN to scale up this intervention among several providers.
Denese Frans-Joseph: I’m so happy to hear how effective your projects have been, you should feel very proud of those impacts. Our next question is about healthcare. Black communities continue to experience systemic barriers in healthcare. From your perspective, what are some of the biggest challenges or pressing issues, and how can research help to address these issues?

Martha Taylor: I believe that one of the most pressing issues that Black communities experience within the Canadian healthcare system is bias from healthcare professionals, which contributes to poor health outcomes for Black communities. We simply aren’t afforded safety within the healthcare system. For those of us who are able to, we often have to advocate for our health concerns to be heard. But what about those of us who can’t advocate for ourselves? I think this racial bias can be addressed through education that takes healthcare professionals on a journey to unlearn anti-Black racism and adopt racially just practices. The Black Health Education Collaborative launched their Black Health Primer in 2024 which aims to do just that. I contributed to its development, editing and copyediting!

Jolen Kayseas: I think as Black people, we know that there’s a long history of medical racism and how that has led to very deep mistrust of medicine, healthcare facilities, and research in general, for example the Tuskegee Syphilis Study. I also think of the social determinants of health and things like redlining that go on within Canada. That also includes inequitable structures like barriers to employment, housing and food security that have greater impacts on Black folks’ health than others. Unfortunately, I don’t think they’ll ever go away, but there are definitely ways that we can mitigate it. Like community based participatory research. That’s one thing that I’m really happy to be involved with on this team. They really are advocates for having researchers with lived experiences join in on not only the data collection, but also contributing their thoughts around analysis and mitigating biases. I also truly believe that we need to have culturally competent training and policies led by Black leaders, Black people and allies to inform healthcare centres and also research centres on how to integrate cultural competence into patient and family care.

Wale Ajiboye: Our healthcare system is set up in a way that sometimes promotes anti-Black racism. Once that is present, it becomes very challenging for Black folks to access or be retained in care. I’ve had some personal experience as an individual, and I will share this example. I went to see my family physician. And I told her my complaint, and she just said, ‘Okay, I’m going to write this medication for you.’ As a healthcare provider myself, I know that there are at least two major investigations or tests that my physician was supposed to do, but she didn’t bother. I asked her about it, and then she realized that I had an understanding of my condition. She then said, ‘Oh okay, yeah, I will send you to do this and do that, and afterwards we can talk once I have the result.’ So that made me to lose respect, and lose trust in in the provider because I felt maybe it was because of my skin colour. I didn’t feel that I was actually adequately taken care of. Those are the types of things that I hear from a lot of members of the Black community. So my research is addressing that, by developing interventions that address anti-Black racism.
Christina Salmon: How has your identity and lived experience as a Black professional shaped your approach to research and advocacy?

Martha Taylor: My experience and identity as a Black professional has shaped my approach to research and advocacy because I always strive to centre the communities I’m working with. Time and time again, we have seen the harm that’s caused when the needs and best interests of communities aren’t prioritized, much less considered. So when I engage in research or advocacy work, I never assume that I know more than the communities I’m working with. I’m there to first understand their concerns and needs, and see how I can work to support and amplify their voices. Communities you are aiming to serve should still have their agency.

Jolen Kayseas: I think lived experience and different intersectionalities are such vital forms of knowledge, I believe approaches such as community-led research can drive equitable changes. So I want to use my lived experience to really drive change for Black people, for Indigenous people and for future generations. I also feel like research often focuses on disparities and hardships that Black people face, and I’m an advocate for highlighting the resilience and the beauty and strength that we have despite the adversities.

Wale Ajiboye: I think for me, lived experience has helped me to approach my work with passion and knowledge. Passion from the perspective of a particular lived experience that I had several years ago, losing a community member, a church member, to HIV. It was based on medical mistrust, because initially he was on HIV medication, and after a while, I don’t know what happened, he stopped taking his medications. And eventually he died. So that really instilled passion in me to ensure that at least people are adequately and well informed in terms of the benefits of HIV prevention tools and also HIV treatment. My lived experience and my identity have helped me to improve the design of interventions to improve uptake of HIV prevention tools. Usually, the mainstream research approach is from the perspective of whiteness. And most times they don’t take cognizance of the fact that Black people have different contexts in which health disparities take place. If you design interventions from the lens of white people, it is not going to work for Black people. You need to understand the context in which disparities develop in Black people, and that it is not so much behavioral, it is more systemic and structural. Having that lived experience helps me to be able to design interventions that work specifically for Black people. It’s been very exciting, using my identity and my deep experience to inform the work that I do.
Denese Frans-Joseph: Wale, I’m so sorry to hear about the loss of your church member. I can connect with that because it’s usually a personal experience for many of us, or it is our lived experience that pushes us to do this advocacy work and do this research to ensure that our communities don’t have to experience the barriers and experiences that we know are so common, right? Thank you for sharing that. The next question I have is around joy. Black joy is a powerful form of resistance and resilience. What brings you joy and how do you incorporate it into your work and daily life?

Martha Taylor: I must say that Black joy is a term I absolutely love, because it truly is our ultimate form of resistance and defiance in the face of systems that have been designed to make us feel anything but joy. Many things in life bring me joy, I’m a very happy person. I love baking, cooking, watching anime, going out with friends, exploring new parts of Toronto, buying shoes, writing fiction and appreciating beauty in everyday life. I believe I incorporate this in my work life because I’ve been told by colleagues that I’m a very sunny and happy person. My joy is something that I carry everywhere I go.

Jolen Kayseas: When I was thinking of that question, I just kept thinking of the Grammys that just happened. You know, a Black woman, Doechii, winning Rap Album of the Year, and Beyonce winning Album of the Year for a country album. Just celebrating Black excellence and creativity and being able to connect with other Black people through that. I feel like we all have a connection based on what we go through living life as Black people. We’re able to empathize with each other and understand each other just based on that. So even just being here in Ghana, I’m with other Black researchers, we’re a completely Black team doing research concerning Ghanaian youth and education. It’s just so great to be surrounded by Black people. That just brings me a lot of joy.

Wale Ajiboye: I think what brings me joy is knowing that what I do ultimately solves problems and also helps Black people and society in general. It’s not just only about Black community, there’s no reason why everybody cannot thrive together. That brings me joy and a lot of energy.
Christina Salmon: I loved your answers so much, thank you. This is our last question. What advice would you give to the next generation of Black researchers and health equity leaders?

Martha Taylor: To the next generation of Black researchers and health equity leaders: we need you! You belong here! Your presence, your voice, your experiences are valid and needed. Hold your head up high and know you are worth it. Your insights are needed. You deserve to take up space. Find your community and your allies, they will help to support you especially when the going gets hard. I’m always rooting for your success!

Jolen Kayseas: I really do believe in challenging the status quo and pushing back and not being afraid to ask questions. What things do you feel are inequitable, pertaining to policies and frameworks? And also promoting rest. You don’t always have to be on the front line. You have allies. I think we were talking about this a couple of months ago, Christina, when you told me that – we have allies who can use their privileges to push change. That really stuck with me. Seek community members, mentors, allies who share the same values. If it wasn’t for my network, I don’t know what I’d be doing right now. My network really helped me navigate challenging times and challenges that I faced, and being able to reach out to folks who understand. So I definitely think that’s important. And being unapologetically Black as well!

Wale Ajiboye: Yeah, thank you, Jolen. Regarding Black researchers, from my own experience, I think the first thing is that you should know what you want and stick with it. There will be so many distractions because of the systemic barriers. For Black researchers, there is this tendency to be distracted and to lose focus. You know, chasing what you think may be the best opportunities for you to break the systemic or the structural barriers. You must first of all identify what you want, and let it be from your own internal reflection and not to just what the opportunity that is available out there, otherwise you will just become a pawn and less effective. So let it be from something that is within you. Once you identify what you want, I think the next thing is to try and communicate it to people around you, because as a Black researcher, you are likely to face systemic barriers. You have to keep talking. You have to keep engaging and to just let people know what you want. The other thing is patience. I think that’s very generic to everybody. You’ve got to be patient, but not sluggish. Persistence. You are patient, but you are not giving up. The last one is to avoid disruptions, because there will be so many disruptions, and don’t let whatever structural barriers you face build up sentiment and hatred within you, because that sucks out energy. Just be focused on your goal and keep preparing yourself, because those opportunities will show up, and you don’t want to be found lacking or wanting.
Denese Frans-Joseph: Thank you so much all three of you. We do have to be clear about what we want, and be unapologetically Black. I think that is the key in all that we do.
Christina Salmon: Thank you all for your teachings and your wisdom. This has been very grounding and inspiring!
Director’s update: MAP’s 2024 year in review
As 2024 comes to a close, let’s celebrate the wins. MAP is an academic research centre with the primary strategic goal of driving system and policy change for health equity. This year we saw sound, scientific evidence, and in no small part MAP research, embedded in several policy gains that promise to yield real, concrete benefits across our lifetimes.
For example, national pharmacare has been a long journey in Canada, with MAP in many ways drawing the roadmap (more on that below). I’m overjoyed to see this crucial building block of health equity begin to come to life.
In 2024, the federal government announced a National School Food Policy and $1B commitment to addressing food insecurity for 400,000 students across Canada. MAP was part of the first national roundtable to inform this work.
Thanks in part to MAP’s national OurCare initiative (see below), many provinces also strengthened their commitments to improving primary care access. Ontario and PEI in particular set goals in 2024 for 100% of their population having access to primary care.
In 2024, we also saw some concerning steps backwards for health equity in Canada, particularly, the loss – rather than the improvement – of research-based, lifesaving harm reduction programs and initiatives in Ontario and BC. These are important reminders that gains can be abruptly lost. There is still a great deal of work to do.
Let’s be energized by the wins. As you read through the impact stories below, I hope you feel proud of what has been made possible with your support. Remember that real change is possible, and it takes time. As always, implementation is everything. We will continue to work with our policy partners to help set these recent wins up for long-term success in the months and years ahead.
Together, we can create a healthier, more equitable future – a future that includes everyone.
Sincerely,
Dr. Stephen Hwang
Director, MAP Centre for Urban Health Solutions
Canada Research Chair in Homelessness, Housing and Health
2024 Research Highlights

A giant leap for universal pharmacare: In spring 2024, the Liberals and NDP reached a landmark and long-anticipated agreement on pharmacare, moving forward a bill that was strongly influenced by MAP research. The bill became law on Oct. 10, allowing Canada’s federal government to begin working with provinces and territories to implement a “first phase” of national universal pharmacare, providing free access to diabetes medication and contraceptives. For MAP Scientist Dr. Nav Persaud, this historic year of progress is the culmination of many years of research, partnerships and advocacy – and there is more work ahead. In November, the federal government named Dr. Persaud the chair of a committee to advise the government on the next steps of the program, including recommendations for expanding to a universal, single-payer pharmacare program. That report will be submitted to parliament in late 2025.

A recipe for more effective, more accessible primary care in Canada: MAP launches the OurCare Standard: In 2023, MAP led the largest-ever public consultation on primary health care, collecting input and ideas from close to 10,000 people across Canada. In 2024, we distilled what we heard into the groundbreaking OurCare Standard: six simple statements that describe what every patient in Canada should be able to expect from primary care. The Standard represents a concrete and achievable vision and a new benchmark for assessing the quality of primary care in Canada. It’s already empowering policy-makers and the public to compare different models of primary care and take steps to improve them. For example, the Connected Care for Canadians Act directly addresses the fourth OurCare Standard.

MAP and Staples Canada launch national awareness campaign: To mark the fourth year of our Even The Odds partnership with Staples Canada, Staples and MAP launched a national mass media campaign called ‘Close the Gap’ to highlight the real health challenges faced by disadvantaged communities across the country. The campaign ran on television, digital, outdoor signage and in Staples stores, and in 2024 garnered more than 100M impressions. Since the launch of Even the Odds in 2021, Staples has raised more than $7M for MAP research.

MAP x APPLE Schools improves health for thousands more kids in 2024: APPLE Schools is an internationally recognized best practice that has been proven to help kids move more, eat better and feel happier – erasing many of the long-term health effects of childhood poverty. MAP’s implementation and evaluation of the award-winning program continues in Ontario and Alberta, and reached 4,500 kids in disadvantaged neighbourhoods in 2024. Watch the program’s cute year-end video highlighting just some of the ways that APPLE Schools promote elementary students’ health.

Divided city: MAP and The Local produce first-ever map of life expectancy across Toronto: Through a unique collaboration with The Local magazine, MAP showed that life expectancy varies by almost 12 years across Toronto neighbourhoods, with residents of the wealthiest neighbourhoods most likely to live the longest lives. The results are captured in interactive maps that reveal stark disparities among neighbourhoods separated by just a few TTC stops, filling a critical gap in our understanding of urban inequality in Canada. Since publication, the City of Toronto has initiated discussions on how we can make these data a regular part of how the city monitors progress on health equity.

Science to drive solutions for a lethal public health crisis: MAP leads the country in research on the opioid crisis. In 2024, we helped Canada better understand the barriers to addiction treatment in Canada and some of the populations at highest risk. As controversy around supervised consumption dominated headlines, the Lancet published our first-of its-kind study to track how supervised consumption sites reduce overdose rates at a population level. MAP was part of a Unity Health Toronto review that concluded supervised consumption should continue but with improved community safety supports. When Ontario announced supervised consumption closures, we moved quickly to quantify the expected impact on the lives and health of people who use drugs, and spoke out to share evidence on the crucial role that supervised consumption plays in an effective public health system.

MAP leads first study of its kind on police funding, featured in New York Times: Policing is the single biggest expense in most Canadian municipalities, but is spending more on policing an effective strategy for reducing crime? A study led by MAP’s Upstream Lab asked this question and found no consistent relation between police funding and crime levels across 20 Canadian municipalities, including Vancouver and Toronto. The findings – more police spending does not mean safer cities – were covered in Canadian national media as well as The New York Times.

MAP leads first-ever Mpox vaccine trial, published in BMJ: Published in September in one of the world’s leading medical journals, MAP’s landmark study was the first-ever emulation of a target trial to evaluate the real-world effectiveness of a Mpox vaccine during an outbreak. Just as WHO declared Mpox a global health emergency for the second time in two years, the study demonstrated the power of today’s vaccine: a single dose can prevent infection.

MAP homelessness research makes headlines: Several MAP studies on homelessness and health made national headlines this summer, raising awareness and guiding urgently-needed policy and practice change. In August, MAP proved that homelessness shortens life by almost two decades – and the disparity in mortality between Canada’s homeless and housed populations is getting worse. In July, the front page of The Globe and Mail featured a MAP study on the value of mandating hospitals to record homelessness among patients; it improves health outcomes through tailored patient care. In June, MAP and the Ontario Drug Policy Research Network released a report that showed opioid overdose deaths in Ontario’s shelter system more than tripled during the pandemic. The report pointed to crucial missed opportunities for intervention: nearly half of those who died had an encounter with the health-care system in the week before death, and 90 per cent had sought help for a mental-health condition.

Innovation and cross-sector collaboration to prevent homelessness, address violence: After years of intense preparation and planning, MAP and Mission Services of Hamilton launched Safe at Home Hamilton in May 2024 – a groundbreaking program to better serve women-identifying and gender-diverse people who are experiencing violence at home. The Safe at Home model requires the perpetrator to leave the family home, giving survivors of violence and their children the option to safely remain in place and recover with supports from integrated health, social, police, and legal services.

Smart vending machines continue rollout across Canada, impact grows: MAP’s Our Healthbox program is now active in 11 communities across Canada and has reached more than 7,000 people, delivering almost 1,000 free HIV self-test kits, more than 1,500 Naloxone kits and 23,000 sexual health items and other supplies to reduce harm. One of our 2024 launches was in Tobique First Nation, New Brunswick – learn more in this great video by Healthbox funder and partner, Staples Canada.

MAP distributes monthly food vouchers to 400 low-income Ontarians: Healthy Food Prescription is a research trial to address food insecurity and chronic disease inequities through a novel and promising approach: grocery store vouchers prescribed by physicians to low-income patients with diabetes. Through a randomized controlled trial, MAP is supporting the health of 400 diabetes patients, and tracking how well the vouchers work to reduce participants’ healthcare use as well as overall risk of diabetes complications. Our goal is to guide governments in the best ways to shift investments upstream and to create better health outcomes for people with low incomes. This goal has never been more urgent; for example, the City of Mississauga and the City of Toronto have both declared food insecurity a state of emergency.

MAP’s awards and recognition continue to grow: MAP scientists and staff are national and international leaders in their areas of research, and in 2024 our accolades were many. In November, the federal government named two new Canada Research Chairs at MAP in the areas of Homelessness, Housing and Health as well as the first-ever CRC in Indigenous Women’s and Two-Spirit Mental Health and Homelessness. MAP is now home to nine prestigious Canada Research Chairs in total. In 2024, MAP scientists were also awarded two St. Michael’s Hospital/University of Toronto chairs, the King Charles III Coronation Medal, the Canadian Medical Association Award for Young Leaders, the University of Toronto Michael Gordon Award for Humanism in Medicine and William Goldie Prize, two Anthem Gold Awards, the CAHR-CANFAR Excellence in Research Award, three Research Mobility Awards from the Emerging and Pandemic Infections Consortium as well as the Future Leaders Prize, a PSI Mid-Career Knowledge Translation Fellowship and the IHSPR-CAHSPR article of the year – to name a few!
Want more research updates?
Subscribe to MAP’s Junction e-newsletter for short, monthly updates on our studies, our solutions, and the issues we study. You can also follow MAP on LinkedIn, and subscribe to our MAPmaking podcast.
Ontario’s second ‘smart’ harm reduction dispensing machine launches in Peterborough
Program led by St. Michael’s Hospital to dispense free HIV self-testing kits, harm reduction, sexual health supplies
April 9, 2024
A machine that dispenses free self-testing kits for HIV and COVID-19, naloxone kits, new needles, condoms and other essential harm reduction and sexual health supplies has launched in Peterborough, Ontario. This will be the second machine in Ontario and connects with the network of communities in New Brunswick and Manitoba.

The ‘smart’ harm reduction machines, called Our Healthbox, work like a vending machine, and also provide health information and a service directory for people to find much-needed health care and supports right in their community. The initiative, led by researchers at St. Michael’s Hospital, a site of Unity Health Toronto, launched at the Trinity Community Centre in Peterborough on April 9. This is part of a plan to launch up to 50 machines across Canada in 2024. The goal is to install 100 machines over the next two years, and to evaluate how well they support people with their health needs.
Together, One City Peterborough and Peterborough Public Health with the support of Peterborough AIDS Resource Network (PARN) and are embarking on this exciting journey to help make the Peterborough community more equitable by increasing access to vital resources and supplies.
“One City is committed to making our community safer for everyone: our neighbours who live outdoors, our neighbours who use substances, and for the many whose lives are made more dangerous by society’s stigma, laws and policies,” said Christian Harvey, Executive Director, One City Peterborough. “Partnering with Peterborough Public Health and implementing Our Healthbox to increase access to resources and supplies the community needs, when they need them, feels like an important step in empowering people to define what safety means to them.”
“Our Healthbox will expand access to local services that allow people to take greater control of their health and well-being without the stigma and judgement that may accompany interactions with agencies and systems,” said Dr. Thomas Piggott, Medical Officer of Health/Chief Executive Officer, Peterborough Public Health. “We are thrilled to be bringing Our Healthbox to Peterborough and to foster a partnership with REACH Nexus and all the participating communities across the country. The machine’s ability to collect real-time data will allow us to be more responsive to the ever-evolving needs of our community. This data, coupled with the connection to harm reduction and wellness agencies across the country, positions us well to be implementing evidence-based best practices into our community.”
The initiative continues to help address the rise in new HIV cases in Canada and the country’s opioid crisis, which claims the lives of 21 Canadians each day. Providing access to harm reduction and health care supplies for free to people in spaces they frequent is a strategy experts consider to be key in reaching people who are underserved and who have barriers to accessing testing, harm reduction materials, treatment, care and prevention due to racism, homophobia, stigma and discrimination.
“Everyone in Canada deserves to have what they need, when they need it, to take care of their health. But we know that this is not the case, and so we are doing everything we can to bridge that gap in ways that work for each person in their community,” said Dr. Sean B. Rourke, a scientist at MAP Centre for Urban Health Solutions, a world-leading research centre housed at St. Michael’s Hospital. As Director of REACH Nexus at MAP, he leads a national research and public health group working on how to make sure everyone who needs access to testing (especially those who are undiagnosed), treatment and care for HIV, Hepatitis C and other sexually transmitted and blood-borne infections (e.g. syphilis) can get what they need to stay healthy and thrive.
Our Healthbox is the latest phase of work led by Dr. Rourke to connect those with complex health and social circumstances to testing, treatment and prevention. In 2019, Dr. Rourke spearheaded a cross-Canada clinical trial which evaluated and proved the accuracy of HIV-self tests – Health Canada approved the tests for use in November 2020 based on the results of the trial. In June 2022, Dr. Rourke launched the I’m Ready program, distributing more than 15,000 free HIV self-testing kits across Canada to reach people who are undiagnosed and get them connected to care, with the goal of identifying the factors that affect access to testing and care.
Dr. Rourke and his team will work with local community-based organizations, public health authorities, and health centres to host and maintain the Our Healthbox program. Each agency determines the supplies needed in the machines to serve the people in their community. The east coast implementation of Our Healthbox is funded by Even the Odds, a partnership between Staples Canada and MAP Centre for Urban Health Solutions.
Our Healthbox is funded by the Canadian Institutes of Health Research (CIHR), the Public Health Agency of Canada, the St. Michael’s Foundation, and Even the Odds (Staples Canada and MAP).
About St. Michael’s Hospital
St. Michael’s Hospital provides compassionate care to all who enter its doors. The hospital also provides outstanding medical education to future health care professionals in more than 27 academic disciplines. Critical care and trauma, heart disease, neurosurgery, diabetes, cancer care, care of the homeless and global health are among the Hospital’s recognized areas of expertise. Through the Keenan Research Centre and the Li Ka Shing International Healthcare Education Centre, which make up the Li Ka Shing Knowledge Institute, research and education at St. Michael’s Hospital are recognized and make an impact around the world. Founded in 1892, the hospital is fully affiliated with the University of Toronto.
About Unity Health Toronto
Unity Health Toronto, comprised of Providence Healthcare, St. Joseph’s Health Centre and St. Michael’s Hospital, works to advance the health of everyone in our urban communities and beyond. Our health network serves patients, residents and clients across the full spectrum of care, spanning primary care, secondary community care, tertiary and quaternary care services to post-acute through rehabilitation, palliative care and long-term care, while investing in world-class research and education. For more information, visit www.unityhealth.to.
About MAP Centre for Urban Health Solutions
MAP is a world-leading research centre dedicated to creating a healthier future for all. Through big-picture research and street-level solutions, our scientists tackle complex community health issues — many at the intersection of health and equity. Internationally recognized for groundbreaking science and innovation, MAP has changed the way the world understands the health consequences of social inequality in Canada. Together with our community and policy partners, MAP is charting the way to the world’s healthiest cities: places where people, communities, and the political, economic, social, environmental and health infrastructures come together so that everyone can thrive. MAP is part of the Li Ka Shing Knowledge Institute of St. Michael’s Hospital and is fully affiliated with the University of Toronto. St. Michael’s is a site of Unity Health Toronto, which also includes Providence Healthcare and St. Joseph’s Health Centre. For more information visit: www.maphealth.ca
About One City Peterborough and Peterborough Public Health
One City Peterborough is a nonprofit charitable organization formed in 2019, as a joining of Warming Room Community Ministries and Peterborough Reintegration Services. Built on the belief that everyone belongs, and it is together that we flourish, One City works to create stability and increase wellness. One City continues to focus on working together as a community to promote housing, community safety, and social inclusion in the City of Peterborough, by responding to immediate needs, breaking down barriers among us, and advocating for systemic change. Visit www.onecityptbo.ca to learn more.
Peterborough Public Health is the public health unit serving the residents throughout the City and County of Peterborough, as well as Curve Lake and Hiawatha First Nations. Guided by the Ontario Public Health Standards, PPH offers a wide range of programs and services to promote and protect the health of our community, with a focus on addressing the upstream causes of health and striving for equity. PPH has long supported harm reduction within our community including a needle exchange program (NEP) for over 25 years. Today, PPH continues to manage the local NEP, with the support of Peterborough AIDS Resource Network (PARN) which provides the front-line operations. Visit www.peterboroughpublichealth.ca to learn more.
Unity Health Toronto media contact: communications@unityhealth.to
One City Peterborough contact: Christian Harvey (Executive Director), charvey@onecityptbo.ca
Peterborough Public Health media contact: media@peterboroughpublichealth.ca
“We Defined Each Other:” MAP Celebrates 25 Years
In 1998, St. Michael’s Hospital’s past CEO Jeff Lozon founded MAP during a turbulent time. The hospital was facing a major financial crisis. A forced and highly controversial merger sparked fears and protest among incoming staff and physicians. Yet these two challenges ultimately defined MAP’s mission and unique value, and pushed St. Michael’s to evolve into the national leader it is today.
Stephen Hwang and Ahmed Bayoumi were two of the very first scientists recruited to what was then known as the “Inner City Health Research Unit.” In this reflective and heartfelt discussion, Jeff, Stephen and Ahmed look back at MAP’s beginnings and what it meant to embed an equity-focused research centre within St. Michael’s Hospital.
Listen: Apple Podcasts | Google Podcasts | Spotify | Audible | Amazon Music | Pocket Casts | Email Notifications
Learn More: View a timeline of MAP’s history. Read a Toronto Star piece about St. Michael’s ‘highly political’ 1998 merger with the Wellesley Hospital.
About the MAPmaking podcast
MAPmaking brings you Canada’s leading voices on the health equity issues that affect us all. Together, we will discuss and explore the scientific evidence and real-world solutions that we believe have the potential to transform our country. Our vision is a Canada where everyone has the opportunity to thrive.