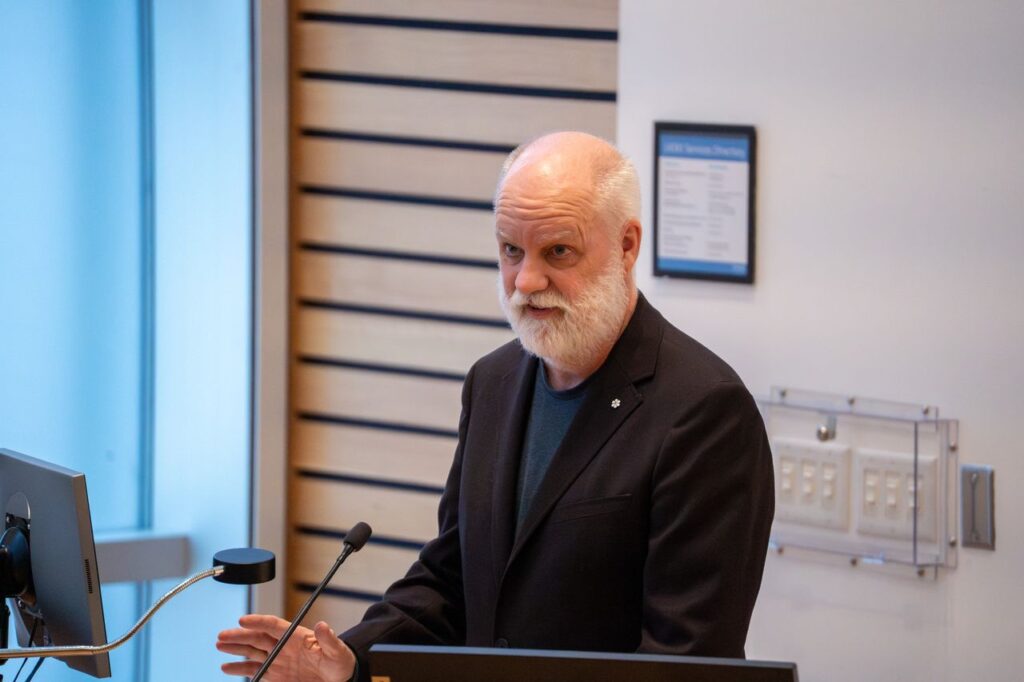
Pictured above, from left to right: MAP Director Dr. Stephen Hwang and MAP scientist Dr. Tara Kiran at the 2025 MAP Solutions for Healthy Cities Symposium, in discussion with Dr. Andrea Tricco (Executive Director Li Ka Shing Knowledge Institute), Stephen Lucas (former Deputy Minister of Health Canada) and Dr. Fahad Razak (Li Ka Shing Scientist).
Message from MAP Director Dr. Stephen Hwang

With 2026 on the horizon, I’m incredibly proud to share some of MAP’s successes from the past 12 months. Some highlights (click here to jump to the full report):
- In Ontario, a new Primary Care Act mirrors MAP’s OurCare Standard, setting ambitious, patient‑centred goals for the province’s health system.
- Nationally, Canada’s first National School Food Program was made permanent in 2025, providing meals to 400,000 children and saving families hundreds of dollars annually.
- Thanks to recent Our Healthbox launches in the Northwest Territories, MAP’s programmatic reach now officially stretches from coast to coast to coast.
- MAP was spotlighted in more than 100 media features and published more than 250 peer-reviewed papers, leading and defining the conversation on what a healthier Canada can look like.
Through each of the stories above and below, I see MAP’s core values in action: world-class research to strengthen Canada’s policies and practices; community partnerships to bring evidence-based health innovations to the places they’re needed most; and a deep commitment to put equity and respect for lived expertise at the centre of everything we do.
These stories also underscore the importance of persistence. Many of this year’s wins were years in the making.
On behalf of MAP’s leadership, researchers, staff and students: thank you to MAP’s many community, academic and policy partners and to MAP’s visionary donors and funders.
Step by step, we are charting the course toward a healthier, safer and more inclusive Canada. Our successes are only thanks to your partnership and commitment. We are grateful to do this work with you.
Sincerely,
Dr. Stephen Hwang
Director, MAP Centre for Urban Health Solutions
Canada Research Chair in Homelessness, Housing and Health
2025 Research Highlights

Canada’s first National School Food Program: Permanent federal funding, local implementation: In 2024, MAP’s Dr. Katerina Maximova helped develop Canada’s first-ever National School Food Program. In 2025, Prime Minister Carney announced that the federal government is making the national program permanent. At the local level this year, Dr. Maximova served on Toronto’s Universal Student Food Program Steering Committee which developed the city’s vision and strategy for universal school meals. City Council unanimously adopted the plan in June. The city will now provide a morning meal in all Toronto school communities by the 2026/27 school year and introduce a lunch program by 2030.

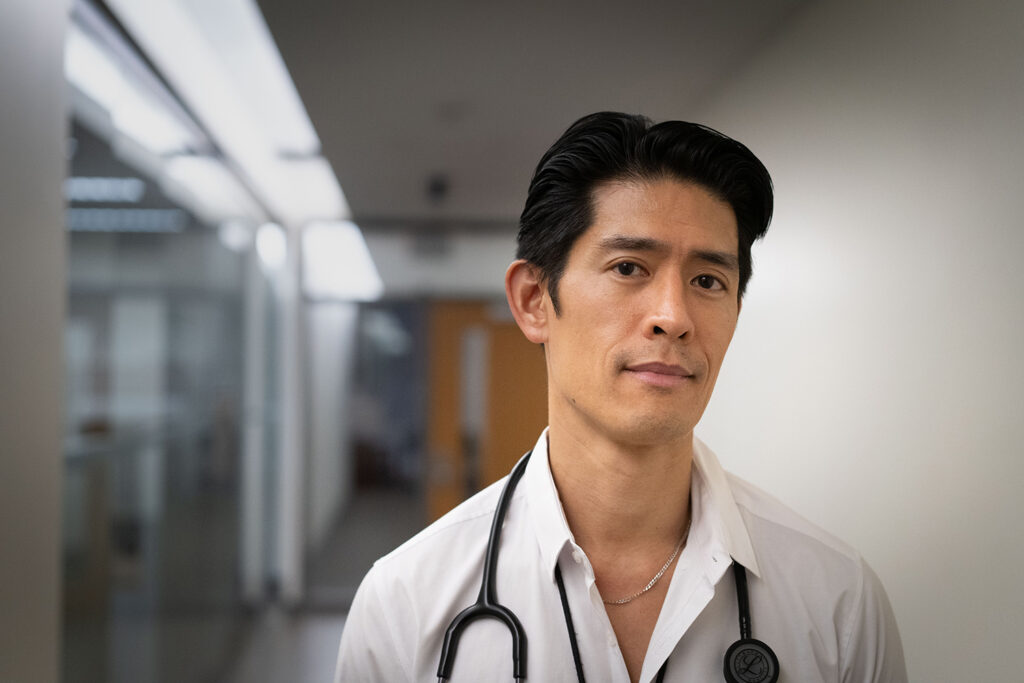
Historic primary care act based on MAP recommendations: In June, the Ontario government introduced the Primary Care Act, a framework of six ambitious, patient-centred objectives for Ontario’s primary care system. The framework is an almost word-for-word reflection of MAP’s OurCare Standard. Watch here as OurCare lead Dr. Tara Kiran reflects on what this means for patients. Dr. Kiran just wrapped up a second phase of the OurCare study (learn more: The Globe and Mail, Toronto Star) and continues to champion implementation of the OurCare Standard nationwide.

MAP reaches the far north, distributes lifesaving supplies across Canada: Since MAP’s first Our Healthbox smart vending machines launched in 2023, MAP has now distributed almost 2,000 free HIV self-tests, more than 37,000 harm reduction supplies and almost 4,000 Naloxone kits — reaching 15,700 people in 22 communities across Canada. In 2025, the program continued to expand with new Healthboxes in New Brunswick (Miramichi), Ontario (Toronto, North Bay), Manitoba (Winnipeg), Alberta (Piikani Nation) and the Northwest Territories (Behchokǫ̀, Hay River, Inuvik and Yellowknife).

MAP drug checking initiative receives $3M of new federal funding, protects thousands across Ontario: In 2023, MAP received $2M of federal funding to create Ontario’s Drug Checking Community, an expansion of MAP’s public health and safety program, Toronto’s Drug Checking Service. This October, Health Canada committed an additional $3M to the program with the goal of establishing a collection site in each of Ontario’s 29 public health unit jurisdictions by December 2027. The service prevents overdose and saves lives every day by rapidly analyzing tiny drug samples to detect and describe unexpected — and often lethal — ingredients. Results not only inform people who use drugs, but also equip community health workers, public health units, first responders, policy makers and others with vital intelligence about what’s circulating in the unregulated drug supply. Since Toronto’s Drug Checking Service launched in 2019, the program has now checked more than 20,000 samples of drugs and used drug equipment.

MAP’s national partnership with Staples Canada reaches 5-year milestone: Launched in early 2021, Even the Odds is a partnership between Staples and MAP to raise awareness of inequity in Canada and to help create vibrant, healthy communities. Through corporate donations and fundraising, Even the Odds funds MAP research and innovative, evidence-based solutions across Canada — to help make the future fair for everyone. Originally struck as a five-year, $5M commitment, we are thrilled to share that the initiative has now raised more than $8M and will continue through a new, multi-year agreement. MAP is incredibly grateful for Staples’ unwavering vision, commitment and transformative support.

First phase of pharmacare comes to life in BC, Manitoba, PEI and the Yukon: In 2024, Canada passed a new pharmacare law that was strongly influenced by MAP research. In 2025 BC, Manitoba, PEI and the Yukon were the first jurisdictions to sign federal Pharmacare agreements, and will now provide residents with free coverage for contraceptives and some diabetes medications. In November, a federal committee chaired by MAP’s Dr. Nav Persaud published its recommendations for launching and paying for a fully single-payer pharmacare program across the country.

MAP’s Navigator program opens third site in Montreal, reaches 1,000 patients: MAP’s signature Navigator Program pairs hospital patients who are homeless with an outreach counsellor — a ‘Navigator.’ The Navigator gets to know the patient and connects them with the health and social support they need to break cycles of homelessness and poor health, and to move forward in securing housing that works for them. Thanks to Even the Odds (Staples Canada), MAP expanded the program to St. Paul’s Hospital (Vancouver) in 2023 as well as Centre hospitalier de l’Université de Montréal (CHUM) in 2025. This summer, Navigator reached a major milestone: the national program served its 1,000th patient (learn more: CTV Your Morning, CBC).

A new standard for violence prevention and survivor-centred care: The first program of its kind in Canada, MAP’s Safe at Home program has now empowered 52 women and gender-diverse people to end violent situations at home — without facing displacement. Delivered in partnership with Mission Services of Hamilton, this innovative model requires the perpetrator of violence to leave the family home. Survivors and their children have the option to safely remain in place, protected by Safe at Home’s integrated supports from health, social, police and legal services. MAP is now building new partnerships to expand the program and help more people to access safety, stability and support where they live.

MAP initiative identifies hundreds of undiagnosed HIV and syphilis infections, connects to culturally safe care: In March, MAP launched the Ayaangwaamiziwin Centre — a groundbreaking public health response to the alarming rise in HIV and syphilis rates in the Prairies and northern territories. The Centre has already reached and tested more than 2,000 people across Alberta, Saskatchewan and Manitoba, identifying more than 200 previously undiagnosed cases of HIV and syphilis and connecting patients to culturally safe treatment and preventative care. Named after the Ojibwe word for ‘carefulness and preparedness,’ the Ayaangwaamiziwin Centre will soon expand to new sites in the Northwest Territories, Yukon and Nunavut.

MAP rewrites Canadian clinical guidelines for HIV prevention medication: MAP scientist Dr. Darrell Tan led a major update to Canada’s HIV prevention medication guidelines, published in December in the Canadian Medical Association Journal. The new guidelines centre equity and access, and offer Canadian healthcare providers and policy makers the latest insights on how to ensure lifesaving HIV medications are effectively prescribed. A key change: providers are now advised to prescribe PrEP to anyone who requests it — even if patients choose not to disclose HIV risk factors. This shift in practice would remove barriers created by clinician ‘gatekeeping’ and recognizes the realities of stigma and discrimination. Marginalized communities continue to face disproportionately higher barriers to HIV prevention and care.


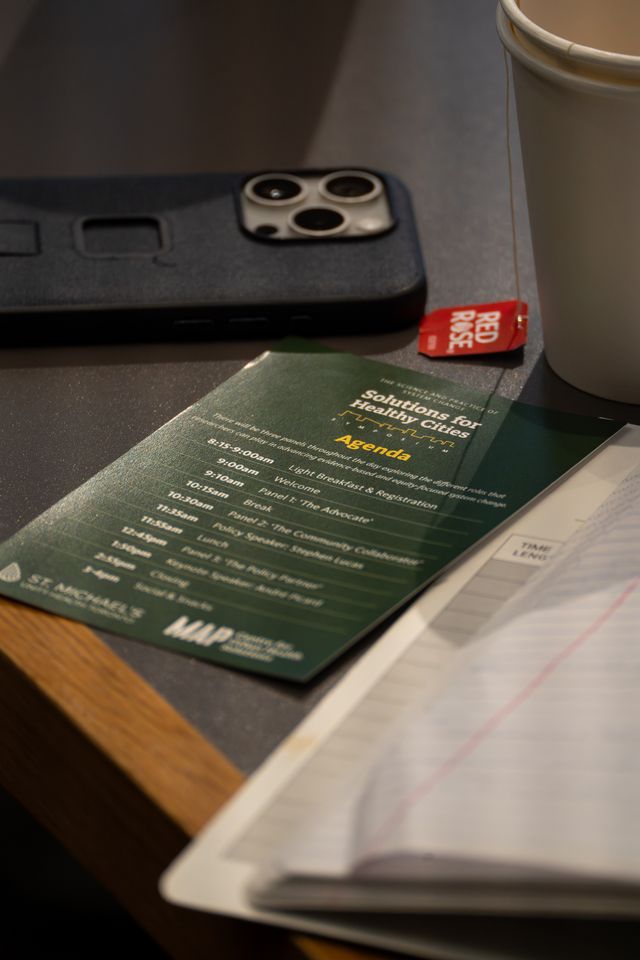
MAP hosts 2025 Solutions for Healthy Cities Symposium: On November 25, almost 200 researchers, service providers, policymakers, students and community experts gathered at St. Michael’s Hospital in Toronto to explore and discuss a multifaceted challenge: how to advance evidence-driven and equity-focused system change in Canada. The 2025 Solutions for Healthy Cities Symposium comprised a full day of talks, discussion and Q&As with policy-focused researchers and insightful guest speakers — including keynote André Picard, one of Canada’s top health and public policy observers and commentators.

MAP x APPLE Schools: Healthier futures for 4,500 more kids in 2025: APPLE Schools is an internationally recognized best practice that has been proven to help kids move more, eat better and feel happier – erasing many of the long-term health effects of childhood poverty. MAP’s implementation and evaluation of the award-winning program continues in 17 elementary schools in disadvantaged Ontario and Alberta neighbourhoods, with plans to expand to reach more students in 2026. What does it look like to be an APPLE School? Here’s an adorable moment with a grade one student, and an example of an APPLE Schools activity that builds movement into the school day.
Primary Focus reaches Top 5 in Apple’s Medicine podcasts, wins international award: Launched in February, MAP scientist Dr. Tara Kiran’s Primary Focus podcast has already gained an active audience in 22 countries, won an eHealthcare Leadership Award and reached the Top 5 in Apple’s Medicine podcast charts. It’s also a finalist for the Canadian Online Publishing Awards in the Best Podcast category. Now in its second season, the podcast brings together the voices of frontline healthcare workers, patients, researchers and policymakers to unpack the issues and innovations that could — and should — transform primary care in Canada.
MAP’s awards and recognition continue to grow: Two out of the three prestigious CIHR Institute of Population and Public Health Trailblazer Awards were awarded to MAP scientists in 2025, recognizing their exceptional contributions to public health research. MAP is also now home to seven Canadian Academy of Health Sciences (CAHS) Fellows (+1 in 2025) and three Government of Canada King Charles III Coronation Medal award winners (+2 in 2025). This year, MAP researchers were awarded the inaugural Royal Society of Canada Eric Jackman Prize, a 2025 Vanier Canada Doctoral Award (Canadian Institutes of Health Research) and two PSI Graham Farquharson Knowledge Translation Fellowships. From the University of Toronto, MAP researchers won the 2025 Peggy Leatt Knowledge & Impact Award (Institute of Health Policy, Management and Evaluation), Louise Lemieux-Charles Health System Leadership Award (Institute of Health Policy, Management and Evaluation), 2025 Doctoral Award (Emerging and Pandemic Infections Consortium/EPIC), Excellence in Research: Mid Career Researcher Award (Department of Family and Community Medicine), Faculty Recognition Award for Exceptional Mentorship — (Institute of Medical Science) and the Dean’s Alumni Award (Temerty Faculty of Medicine). Finally, a MAP collaboration with The Local Magazine won the Jackman Award for Excellence in Journalism at the 2025 Canadian Journalism Foundation Awards.
Want more research updates?
Follow us on LinkedIn and subscribe to MAP’s Junction e-newsletter for short, monthly updates on our studies, our solutions and the issues we study.