The Health Services Restructuring Commission announced that Toronto’s 87-year-old Wellesley Hospital was to be closed, and the bulk of its programs were moved to St. Michael’s. The Wellesley had a strong tradition of caring for people experiencing disadvantage and stigma, including people with HIV infection and those experiencing poverty or homelessness. The merger brought several rising stars to ICHRU, including:
- Dr. Rick Glazier, a family doctor and scientist. Soon after joining ICHRU, Dr. Glazier launched the Toronto Community Health Profiles Partnership, now Ontario Community Health Profiles Partnership.
- Dr. Ahmed Bayoumi, an internal medicine physician with a research focus on HIV care and the care of people who use drugs. Dr. Bayoumi went on to lead and co-lead several pivotal MAP studies, including research that successfully made the case to expand supervised injection facilities in Canada.
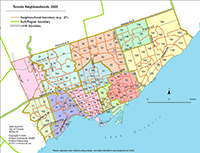
We founded Toronto Community Health Profiles Partnership (TCHPP) to fill an important knowledge gap: community organizations and health and social services providers had little access to urgently-needed, community-level, demographic, socioeconomic, and population health information about the areas and populations they served. In 2005, TCHPP expanded to become Ontario Community Health Profiles Partnership, a publicly accessible, searchable health database and service that many health and community organizations across the province today depend on to help plan and evaluate their programs.
In 1998, St. Michael’s received a donation to establish the Fondation Baxter & Alma Ricard Chair in Inner City Health, the first endowed chair of its kind. The inaugural holder of this Chair was Dr. Donald Wasylenki. Later chairholders included Dr. Pat O’Campo and current chairholder Dr. Ahmed Bayoumi.

We published one of the first-ever papers in a general medical journal describing the links between homelessness, housing and health. The paper was widely recognized as groundbreaking – changing the conversation about homelessness and housing worldwide. It has since been cited in more than 1000 academic publications. In 2014, we published a follow-up to the article, this time in the world’s highest-impact general medical journal: the Lancet. It focused on reviewing evidence-based solutions, and highlighted Housing First as a proven approach to end chronic homelessness.
The Ontario Ministry of Health and Long Term Care announces $8M over four years in infrastructure funding for the ICHRU. The grant was used to recruit more scientists and establish core shared supports. At the end of the initial four-year term, the funding was extended annually until 2014.
Under the leadership of interim Directors Drs. Rick Glazier and Wendy Levinson, the ICHRU attracted new talent from around the world. As the ICHRU grew, its impact expanded: in 2002, ICHRU hosted the first-ever International Conference on Inner City Health, highlighting the unit’s growing global reach. Drs. Bayoumi and Hwang, who co-chaired the conference, published a paper that helped define and advance inner city health as an emerging, complex, and increasingly relevant discipline. “Throughout the research endeavor, the inner-city health researcher must carefully balance the roles of investigator, advocate, activist, and caregiver.”
World-renowned Johns Hopkins epidemiologist Dr. Patricia O’Campo was recruited to be the second holder of the Inner City Health Chair and Director of the Unit, a position she held for 11 years. Dr. O’Campo had authored one of the first papers to examine the social and economic factors that affect health. Her early career research helped shape what is now known as social epidemiology. Today, Dr. O’Campo is a MAP Scientist, Executive Director of the Li Ka Shing Knowledge Institute at St. Michael’s, and a Tier 1 Canada Research Chair in Population Health Intervention Research.
The Unit’s new name was chosen to reflect the Unit’s growth and status as a Centre within St. Michael’s Hospital. The mission remained the same: reducing health inequities through innovative research and knowledge translation to support social change.
Under Dr. Pat O’Campo’s leadership, CRICH launched the 24-month ACHIEVE (Action for Health Equity Interventions) Training Program. Funded by a multi-year, CIHR Strategic Training Initiative in Health Research (STIHR) grant, ACHIEVE trained 38 postdoctoral fellows to generate and apply evidence to address and close health inequities. Alumni went on to be Canada Research Chairs, hospital and university chairs, researchers, professors and leaders at institutions across North America including MAP and Unity Health Toronto.
More than 500 attendees from 19 countries attended, more than doubling the attendance of the conference’s inaugural year.
Recommendations we developed with Stanford University and Duke University were adopted by the U.S. Centres for Disease Control (CDC) to expand HIV screening for all patients 13-64 years in all health care settings. Our economic analysis showed that routine HIV screening for everyone was cost effective and a good use of health care resources, even where prevalence of HIV is low.

The startling results of our Diabetes Atlas, developed with ICES, received widespread media attention, including an interactive website launched by the Toronto Star. The findings informed the Ontario Ministry of Health and Long-Term Care’s 2008 Chronic Disease Management Strategy, and was immediately recognized by the City of Toronto, the Toronto Transit Commission (TTC) and the provincial government as an important guide for policy decision-making. Follow-up research included the Peel Diabetes Atlas and Healthy Development Index.

We were the first to quantify the profound impact that homelessness can have on a person’s life expectancy, proving that homeless men are eight times as likely to die as men in the general population. A large follow-up study, looking at 11 years of national data, found that among those who were homeless or marginally housed across Canada, the probability of survival to age 75 was only 32%. These stark findings were used to advance advocacy and policy arguments across Canada.
CRICH launched a Survey Research Unit (SRU) to support data collection and data quality for equity-focused research projects. Today, SRU clients include researchers and program development staff based in hospitals, universities, research centres and third-sector organizations.
Dr. Stephen Hwang was appointed St. Michael’s inaugural Chair in Homelessness, Housing and Health, the first endowed research chair aimed at better understanding the health needs of people experiencing homelessness.
Now an independent organization, Well Living House was founded at CRICH as an action research centre for Indigenous infants, children, and their families’ health and well-being. Its founder, Dr. Janet Smylie, continues to lead Well Living House and is now Strategic Lead of Indigenous Wellness, Reconciliation and Partnerships at Unity Health Toronto.

We led the Toronto arm of the Mental Health Commission of Canada At Home/Chez Soi study (2009-13), the largest randomized controlled trial in history to evaluate solutions to address homelessness. Our success testing the “Housing First” approach influenced the province of Ontario to set a goal to end chronic homelessness within the next ten years. Citing our evidence, the Ontario Ministry of Health and Long-Term Care also committed to invest $4M long-term funding to sustain housing and support to At Home participants in Toronto, and the federal government committed resources to scale up Housing First interventions across the country.
The Ontario Ministry of Health and Long Term Care announced that it would no longer provide regular infrastructure support to research centres across Ontario, including CRICH. Over the next few years, under Dr. Hwang’s leadership (see below) and with the support of St. Michael’s Foundation and its very committed donors, the centre’s operations successfully transitioned to a philanthropic funding model. With the campaign came a new name for the centre: the Centre for Urban Health Solutions (CUHS).
At the close of Dr. Pat O’Campo’s 11-year tenure, Dr. Stephen Hwang was named the centre’s new Director.
“The arc of my research is the same as the growth of the (research) centre,” said Dr. Hwang. “It started as a tiny enterprise, just me doing little projects. A researcher’s first impulse is to look at a problem and describe it: the (elevated) death rate among the homeless, their lack of access to mental health care. But research has to make a difference in people’s lives.” (Toronto Star)

Our research advanced advocacy leading to the Ontario Ministry of Health and Long-term Care’s life-saving decision to start distributing naloxone to inmates just prior to their release. Our studies showed that 10% of overdoses in Ontario were associated with release from incarceration, and that the highest-risk period was the first few days to two weeks after release – before most people can see a healthcare provider.

Our research exploring the value and feasibility of supervised injection facilities was fundamental to establishing the evidence base for these services in Canada. Public health officials, community groups, and elected officials used our research to support applications to the federal government that resulted in the introduction of supervised injection facilities in Toronto. The Toronto Board of Health relied on these findings to appeal to the Federal Government to relax criminal restrictions on supervised injection.
With refreshed strategic positioning, the centre grows to a team of 20 multidisciplinary scientists managing $30M in health equity research projects.

An advisory council set up by the Liberals proposed a national project to implement a universal public program for prescription drugs. Our first-of-its-kind research was endorsed and cited in the report as as a key resource and starting point for major pharmaceutical policy reform in Canada. In the years that followed, we continued to advance the pharmacare debate in Canada by proving that if everyone in Canada could access essential medications free of charge, it would not only improve the country’s health overall, but would save the health-care system billions of dollars.
To support an ambitious fundraising campaign, the centre updated its brand with the addition of “MAP” to its name, “Centre for Urban Health Solutions.” Why MAP? It’s not an acronym. Instead, it represents our vision and our purpose. Together with our community and policy partners, we are charting the way to a healthier future for all.
MAP launched 10 national, collaborative solutions networks with a common goal: to effect real-world social change by co-designing and demonstrating what works to address critical urban health challenges in our communities. On March 2-3 2020, just days before the COVID-19 pandemic was declared, MAP hosted a symposium in Toronto that brought together more than 170 network members from across the country: scientists, community partners, policy makers, and people with lived expertise.

When the pandemic struck, MAP scientists moved quickly to direct our expertise where it was most needed. MAP created COVID-19 data models to help front-line organizations predict spread in their local, client populations, led COVID-19 clinical trials, and worked to build a better health and social system. We provided expert opinion and informed public health responses in real time. MAP’s research showed that lower-income Toronto neighbourhoods were disproportionately impacted by COVID-19, which led to public policy that prioritized vaccinations for these hotspots. As Canada shifted focus to pandemic recovery, MAP launched a task force to identify the interventions and policy changes most likely to address COVID-19-related inequities in a post-pandemic world.

MAP research was instrumental in winning Health Canada’s landmark approval of the first HIV self-test in Canada: a one-minute, finger-prick blood test that can be purchased online and completed at home. Working together with community organizations, the health sector, and funders including Even the Odds, we are now distributing 50,000 HIV free self-testing kits across Canada through innovative mobile apps that support testing and connections to care, and “smart” vending machines that dispense HIV self-tests as well as free naloxone kits, harm reduction supplies and health information.
Staples and MAP announced a first-of-its-kind partnership called Even the Odds, a three-year, $3-million commitment to raise awareness of inequity in Canada and fund the development of MAP’s program and policy solutions. The partnership has since been extended to five years, and has surpassed its campaign goals thanks to the commitment and support of Staples’ customers, associates, and vendor-partners as well as corporate match donations.

We were among the first to sound the alarm re: the equity implications of Mpox public health responses and related stigma, and the importance of global vaccine equity. We worked quickly to launch and complete a Mpox vaccine modelling study that provided a roadmap for vaccination.
On March 23, 2023, MAP hosted the second Solutions for Healthy Cities Symposium in Toronto. Almost 200 researchers, service providers, policymakers, students and community experts gathered to explore and discuss this year’s theme: the science and practice of implementation success.

In 2016, we were successful in advocating for new municipal policy in Toronto that would open cold weather drop-ins earlier in the season, and allow them to remain open continuously over the coldest winter months. Our 2019 and 2023 studies prompted the City of Toronto to increase temperature thresholds for activating warming centres from -15C to -5C. An evidence-based brief summarizing the research remains one of the most-visited pages on the MAP website.

Health Canada’s Substance Use and Addictions Program (SUAP) announced more than $21 million in federal funding for projects including the expansion of MAP’s multisite Drug Checking Service (a Canadian first) and our groundbreaking DoseCheck technology. This support will expand the life-saving services, promote our provincial monitoring of the unregulated drug supply, and directly contribute to better outcomes for people who use drugs.

MAP is world-leading research centre dedicated to creating a healthier future for all. We are a team of 60 scientists, investigators and postdoctoral fellows and more than 160 staff and students. We are home to six prestigious Canada Research Chairs and more than $100M in active studies. For 25 years we have been central to St. Michael’s mission to serve the disadvantaged and we are proud to remain based in the Li Ka Shing Knowledge Institute at St. Michael’s Hospital, now a site of Unity Health Toronto.
