How have Ontario family doctors’ practice patterns changed because of COVID-19?
COVID-19-related demands and restrictions have dramatically impacted health care in Canada and around the world. This project will help us understand exactly how primary care has changed in the COVID era, particularly the degree to which care has shifted from office to virtual care, and which patients are most affected by these changes in primary care practice.
Using administrative health data collected by ICES, this project will examine:
- How practice patterns have changed – including the volume of care delivered in the office and virtually, and care continuity
- How patterns differ by patient and physician characteristics, by geography, and over time
- What types of care are and are not being deferred
- How many primary-care physicians in Ontario stopped working during the COVID-19 pandemic
We will do this by comparing Ontario’s primary care physician billings data pre-COVID-19 (January 1 to March 10, 2020) to data from the COVID-19 era (starting March 11, 2020). We are also comparing primary care practice patterns during the COVID-19 era to the same period in the previous year (2019).
The results of this work help us understand whether patients with high health-care needs are continuing to receive the care they need to manage chronic conditions. Results will also identify challenges that patients are facing in accessing virtual care, and inequities in access to care (e.g. related to age, health needs, rural vs. urban).
How did primary care practice change after the pandemic?
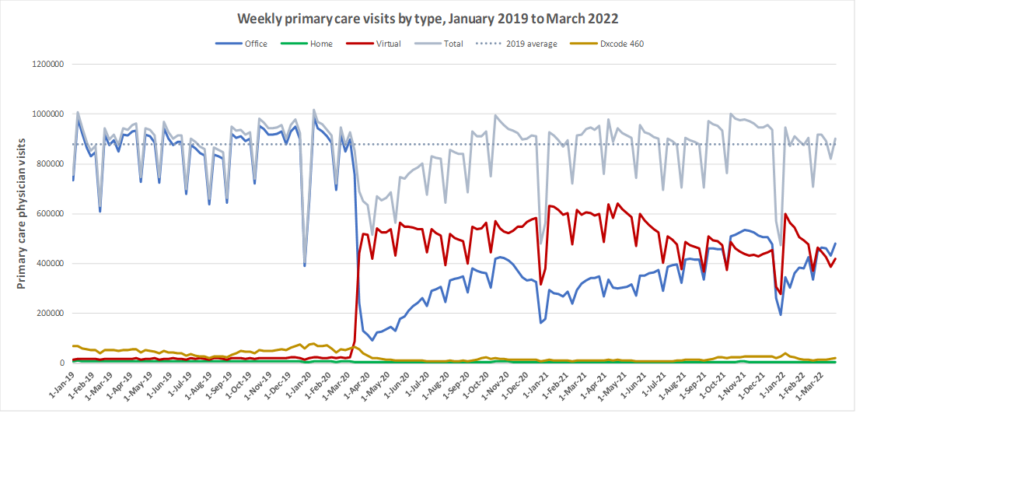
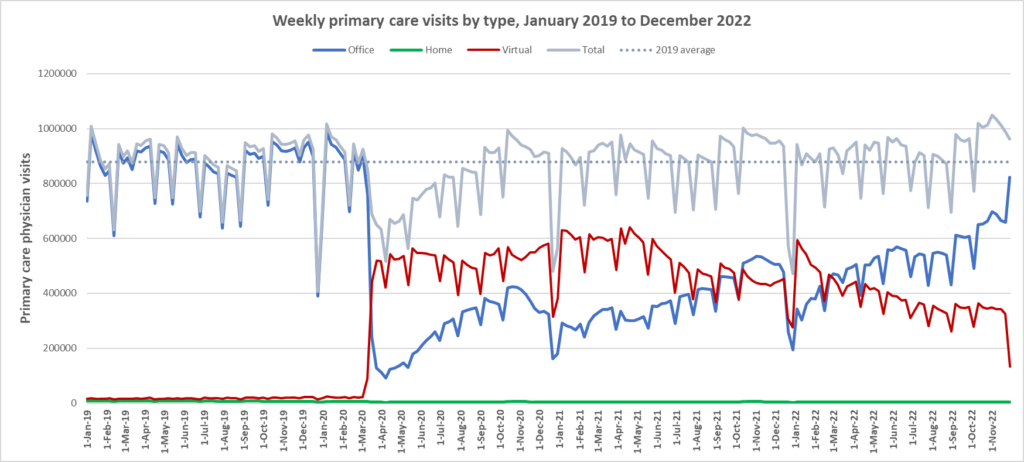
Our initial findings were published in CMAJ in January 2021. We found that compared with 2019, total primary care visits between March and July 2020 decreased by 28.0%, from 7.66 to 5.51 per 1000 people/day. The smallest declines were among patients with the highest expected health care use (8.3%), those who could not be attributed to a primary care physician (10.2%), and older adults (19.1%). Office visits declined by 79.1% and virtual care increased 56-fold, comprising 71.1% of primary care physician visits.
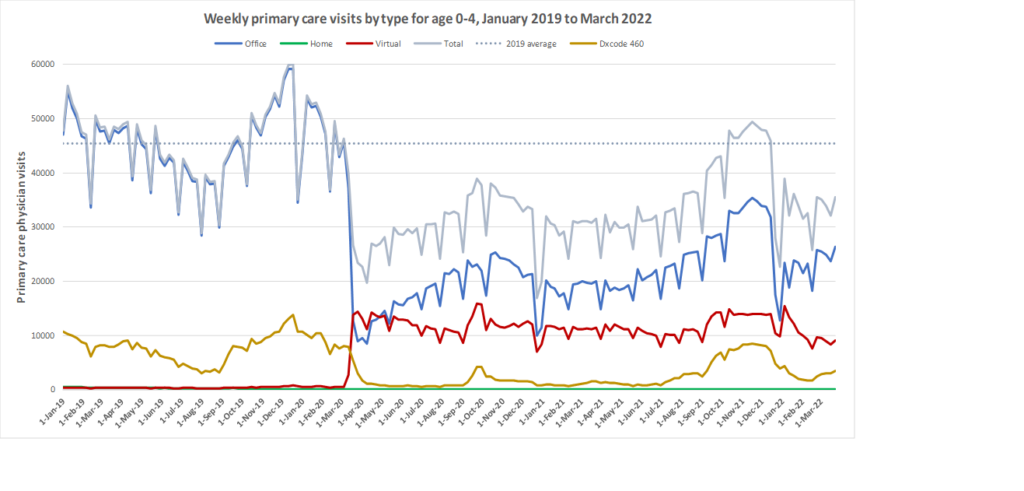
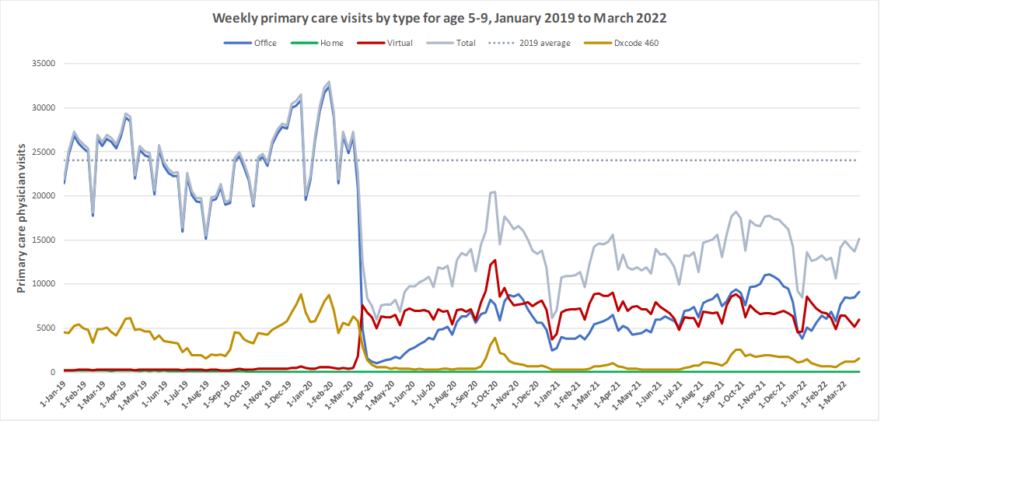
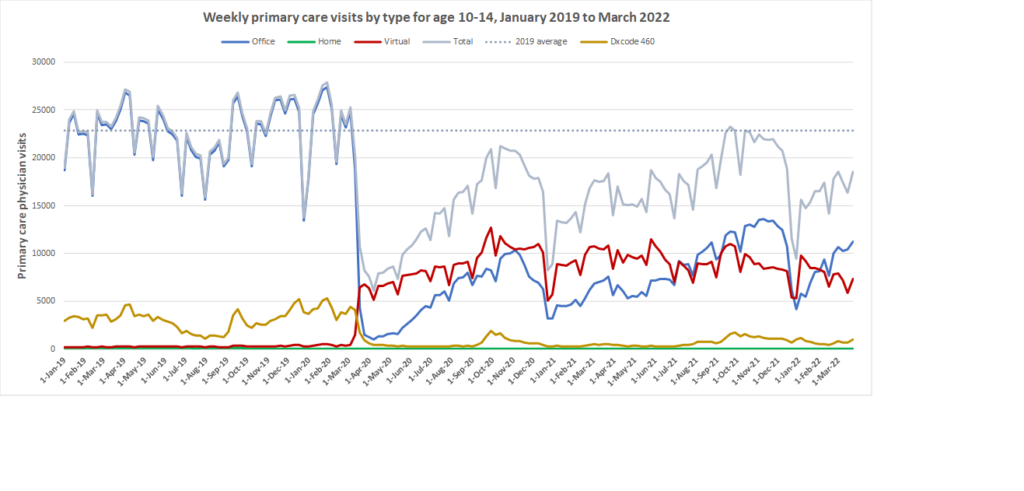
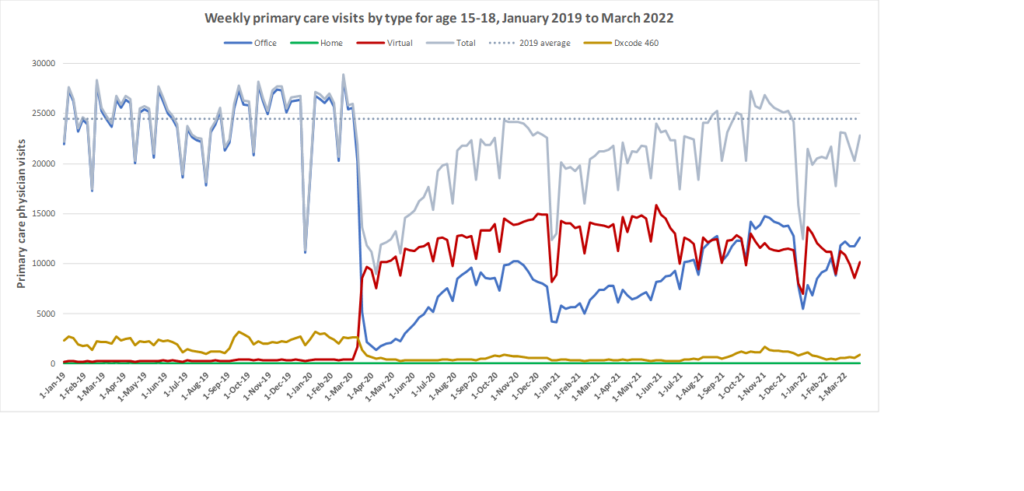
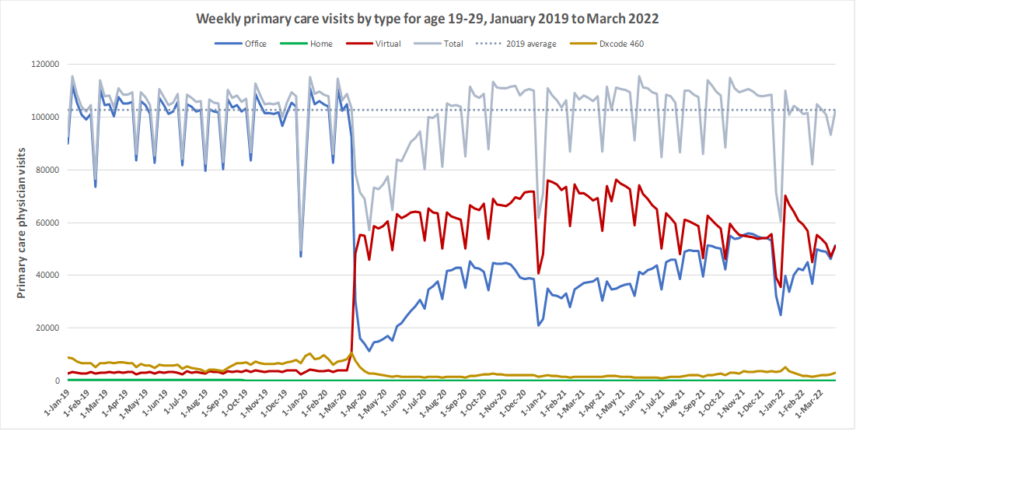
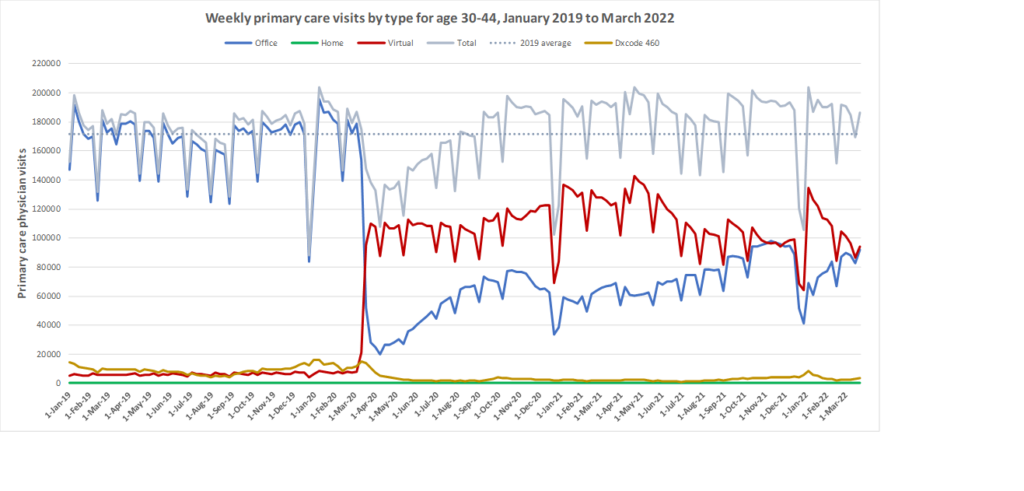
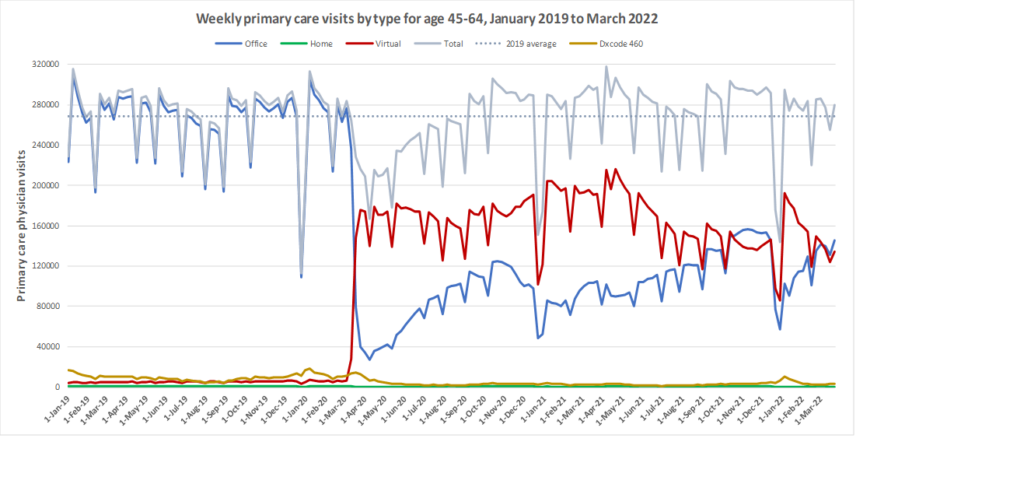
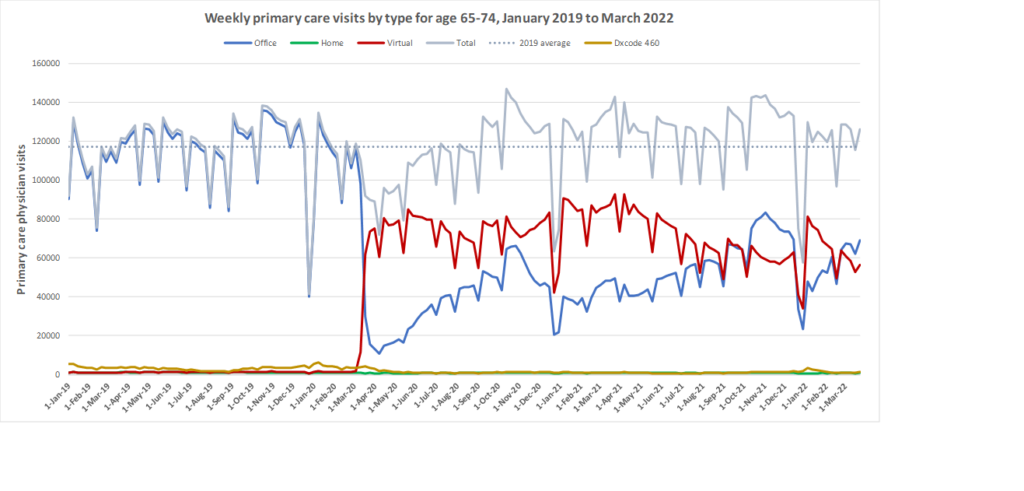
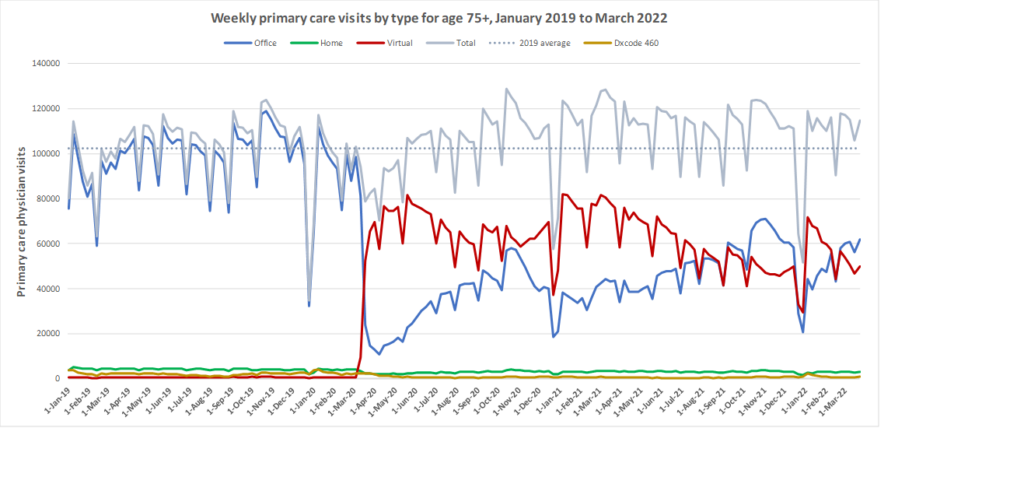
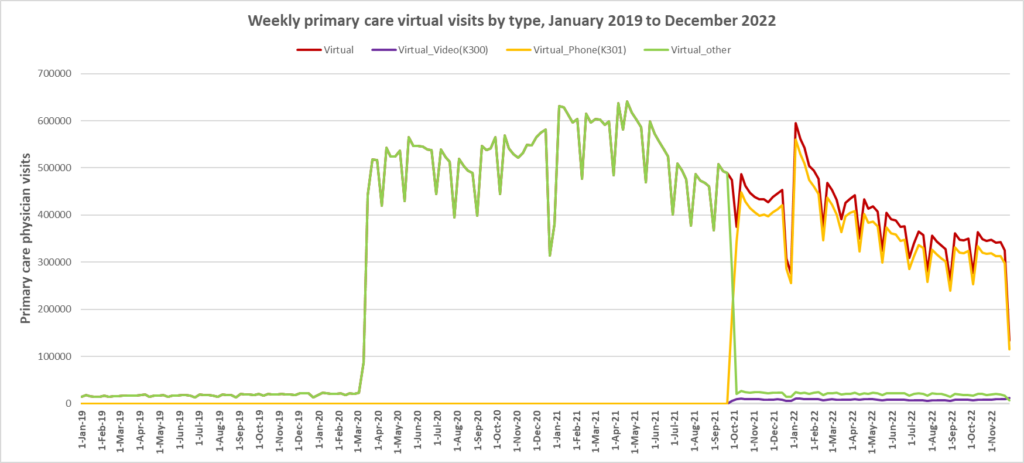
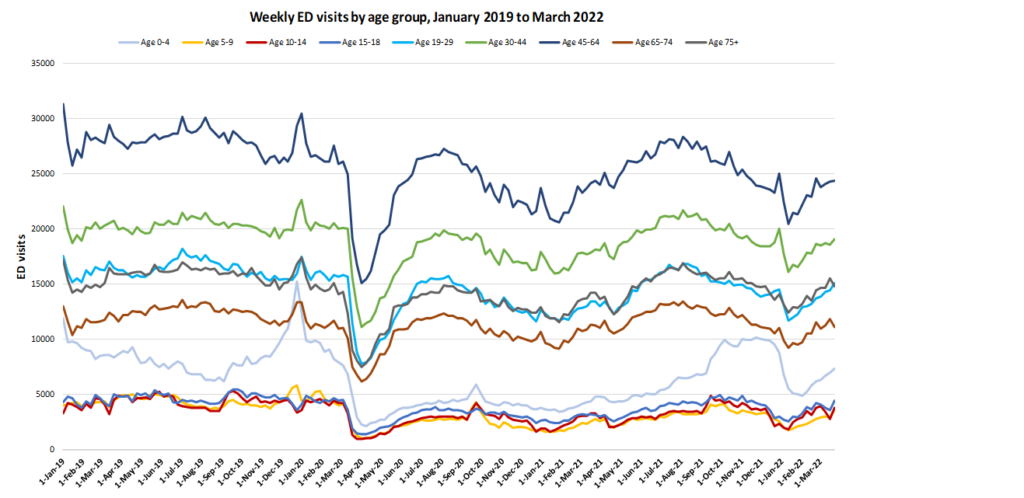
Here are some more up-to-date data. Overall, total visits returned to pre-pandemic levels by Fall 2020 and were maintained at that level through to March 2022. However, there is variation by age. For example, total visits for children have been below pre-pandemic levels since March 2020 while total visits for seniors have been higher than pre-pandemic levels. The reduction in total visits for children and teens may be related to the decrease in non-COVID viral illnesses that usually bring this population to the primary care clinic. In all age groups, a substantial amount of the care continues to be virtual with higher proportions of virtual care occurring during COVID waves. We will be posting updated versions of this graph approximately every quarter.
Did the pandemic cause some family doctors to retire early?
More recent research from our team suggests that twice as many family physicians stopped work in Ontario, Canada during the first six months of COVID-19 compared to previous years. Our findings suggest COVID-19 may have accelerated retirement plans for a subset of older physicians with smaller, fee-for-service practices. The absolute number of physicians stopping work was small, but even still, the impact on patients and communities is likely substantial. Read a pre-print summarizing our work here.
What was the impact of virtual care on emergency department visits?
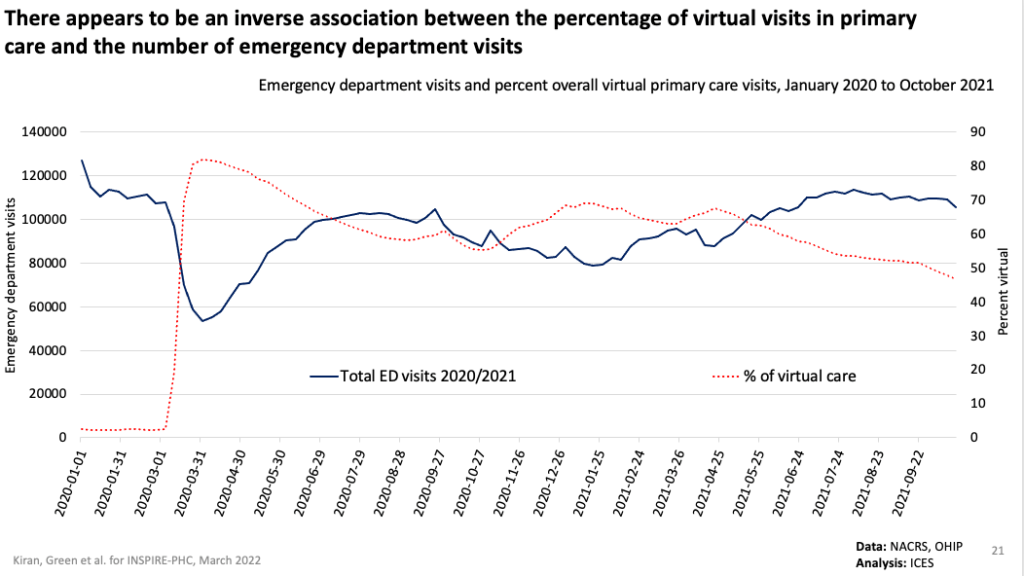
In late summer/early fall of 2021, there were some concerns that family doctors were not seeing enough patients in-person and that this was causing an increase in emergency department (ED) use. However, our preliminary findings counter this narrative. Our preliminary results show that total ED visits from March 2020 to October 2021 were lower than ED visit volumes in 2019. There was no crude ecological association between the percentage of care delivered virtually by family doctors and ED visit volumes (see graph below). Furthermore, patients of primary care physicians providing a high proportion of virtual visits (80-100%) did not have meaningfully higher emergency department visits and any differences pre-dated the pandemic. You can view a summary of our preliminary findings here.
As of March 2022, emergency department visit rates were at or below pre-pandemic levels for all age groups.
Emergency department visit rates remained at or below pre-pandemic levels after a steep drop early in the pandemic
How has the COVID-19 pandemic affected the quality of primary care in Ontario?
Using administrative health data collected by ICES, we examined primary care quality indicators at 6-month increments between October 2018 and April 2022. These primary care quality indicators represent care ranging from cancer screening, chronic disease care, prescribing of high-risk medications, continuity of care and primary care capacity.
Several indicators show a decline in quality after the pandemic and have not yet returned to pre-pandemic baseline, including cancer screening (colorectal cancer and breast cancer), in-person follow-up for patients with diabetes or hypertension, and retinopathy screening for patients with diabetes. We also found that existing income-related disparities in colorectal cancer screening widened during the pandemic.
On the other hand, there are indicators that did not change through the pandemic, including continuity of care (as measured by visits to usual provider of care) and prescribing of statin medications for patients with diabetes. In terms of primary care capacity, we found that although new patient enrolments decreased after the start of the pandemic, they have returned to their pre-pandemic baseline. As well, we found that indicators related to high-risk prescribing (total opioids prescribed, new opioid states, or co-prescribing of opioids and benzodiazepines or z-drugs) improved over time. View our full results here.
Related projects
Keeping Doors Open is a project using survey data to understand changes in family physician practice patterns and what portion have had to close their doors.
In a project based at the University of Toronto Department of Family and Community Medicine, we are also trying to understand patient’s experience and views of virtual care during the pandemic.