Read the study team’s report from the 2019 HPV Symposium: Vaccination in Young GBMSM
Three-quarters of all people in Canada will be exposed to the human papillomavirus (HPV) at least once in their lifetime. While some types of HPV are low risk, other strains cause cervical, anal, and oral cancers.
Vaccines and screening programs to prevent HPV-related cancers are available in Canada, but they’re not easy for everyone to access.
Two populations at particularly high risk of HPV are:
- Gay, bisexual and other men who have sex with men (gbMSM). HPV is very common among gbMSM, impacting 78-98% of this population. Although several Canadian jurisdictions, including Ontario, have a targeted HPV vaccine policy for gbMSM aged 9-26, this requires a young man to be aware of his sexual orientation, and to be willing to disclose it to a provider.
- Men and women living with HIV infection. Research shows that this group is not getting the HPV-related cancer screening they need. The rate of anal cancer among HIV+ gbMSM is 100 times higher than in the general population. Only half of women living with HIV in Ontario undergo regular cervical cancer screening.
How can we make it easier for high-risk groups to access HPV vaccination and screening for HPV-related cancers?
Using a community-based perspective, this project will generate solutions by gathering and integrating scientific as well as community knowledge:
- Searching the scientific literature: We have synthesized findings and recommendations from eight recent research studies about HPV vaccine uptake and willingness, HPV awareness, and screening for HPV-related cancers.
- Consulting with the community: We brought the evidence we gathered to health/service providers and people with lived expertise, to discuss, listen and acknowledge concerns. We then gathered ideas and advice from this community, looking for innovative ideas, alternatives and recommendations for policy and practice.
What we’ve learned so far
Evidence to action: What’s next
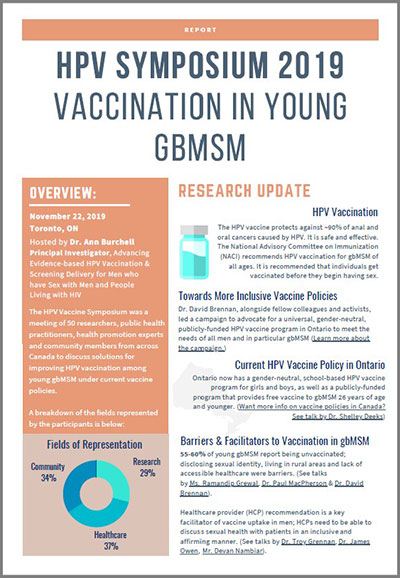
Evidence from the studies included in the grant were synthesized and disseminated by community investigators through several presentations at partner organizations. A national symposium on the topic of HPV Vaccination in Young gbMSM was held in 2019 with invited researchers, health care practitioners, health promotion experts and community members. The goal of the symposium was to inform solutions to improve HPV vaccination among young gbMSM in the context of targeted vaccine policies. A brief overview and report of the findings from this symposium can be found here.
The Engage-HPV study is now examining gbMSM in relation to a ‘vaccination cascade’, where men are divided into four stages: those who are unaware of the HPV vaccine, men who are undecided/unwilling to get the vaccine, men who are willing to be vaccinated and those who are vaccinated. This cascade approach will allow us to understand how men across these stages differ, which can help strategize efforts to improve vaccine uptake and identify subpopulations for vaccine promotion. More research is also needed to understand the significant gaps we identified in HPV literacy among people living with HIV.